Dr Liji Thomas, MD
More than 90% of Hemolytic uremic syndrome (HUS) cases in children are caused by an enteric infection with the Shiga toxin-producing bacterium E. coli (STEC) strain O57 H7. Other strains may also cause STEC but rarely lead to HUS.
The O157 H7 strain infects 1% of healthy cattle, inhabiting the intestine but may contaminate the flesh during normal slaughterhouse processes. It is transmitted to children through undercooked beef, as well as by hand-to-hand transfer by people involved in food preparation and serving, but failing to observe proper hygiene. This results in feco-oral transmission.
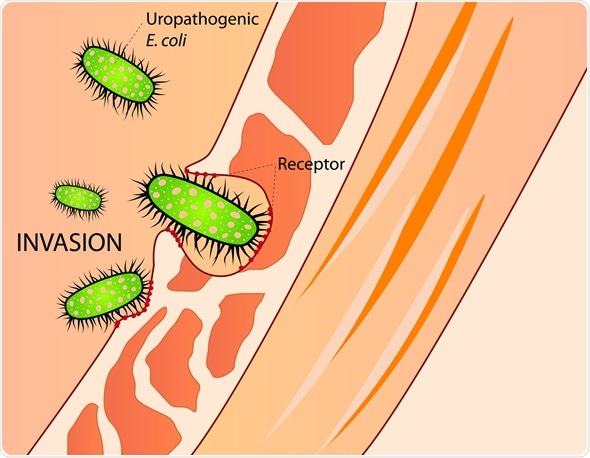
Invasion of E. Coli - Image Copyright: mmzgombic / Shutterstock
Sources of STEC Contamination
Some foods which may spread STEC include:
- Unpasteurized juices or milk
- Undercooked venison, beef, or sausages made from beef
- Non-chlorinated water
- Lake water contaminated with feces
- Certain raw vegetables such as leaf lettuce, alfalfa sprouts and radish sprouts
- Farm animals (through hand contact)
Region-Wise and Age-Wise Distribution
Most HUS cases occur in children between the ages of 1-10 years. Approximately 1-3 cases occur for every 100 000 children in this age group, and in most cases it is self-limited. However, the age characteristics differ between regions. Thus Europe and North America report the highest incidence of diarrhea-associated HUS was in in the 1-5 year age group, while an Argentinian study showed that the very young children (6 months to 4 years) were the most affected.
The incidence is somewhat higher in warm seasons with peak incidence between June and September. HUS following diarrhea may be endemic in some regions. Colder regions have a higher incidence of the disease compared to warmer climates. The incidence varies from country to country.
Risk Factors for HUS
Among those infected with STEC and who develop diarrheal illness, only 3-15% will progress to HUS. Those at risk for HUS in this group include:
- Young children
- Immunocompromised individuals
- Those in contact with infected farm animals
- Those with bloody diarrhea
- Those with fever associated with STEC infection
- Those with a high white cell count and CRP levels
- Those exposed to antibiotics, or antidiarrheals in early acute infection – perhaps because of prolonged exposure of the gut to the bacterial toxins
In idiopathic HUS, pregnancy or exposure to calcineurin inhibitors may precipitate the development of the syndrome.
Microbial Profile
In most parts of the world where HUS occurs, the E. coli serotype O157:H7 is commonly associated with HUS. This includes:
- North America
- Japan
- Western Europe
- South America
- Africa
Sporadic disease is the most common form of D+HUS, but endemic outbreaks, often traced to cattle or sheep reservoirs of the bacterium, have occurred. These are often because of the consumption of food which has come into contact with animal feces in some way, and become contaminated with the organism.
Other strains have also caused large outbreaks of D+HUS, such as E. coli O104:H4, O26:H11/H-, O157:H-, and O145: 28/H-. In rare cases, O103/H2/H-and O111/H8/H are involved. In Australia, large and virulent outbreaks have been caused by O26 H11 H- which produces both Shiga 1 and 2 toxins.
Apart from STEC E. coli, Shigella dysenteriae, and Citrobacter freundii are also known culprits in this condition.
References
Further Reading
Last Updated: Feb 26, 2019