What makes S. aureus so dangerous?
Adhesion and invasion of host tissues
Toxins and enzymes: Tools for survival and spread
Immune evasion mechanisms
Clinical impact
Antibiotic resistance: The rise of MRSA
Staphylococcus aureus (S. aureus) is one of the most prevalent and clinically significant bacterial pathogens. Its ability to survive and thrive in diverse environments, particularly within the human host, is largely due to its remarkable adaptability and a broad arsenal of virulence mechanisms.2
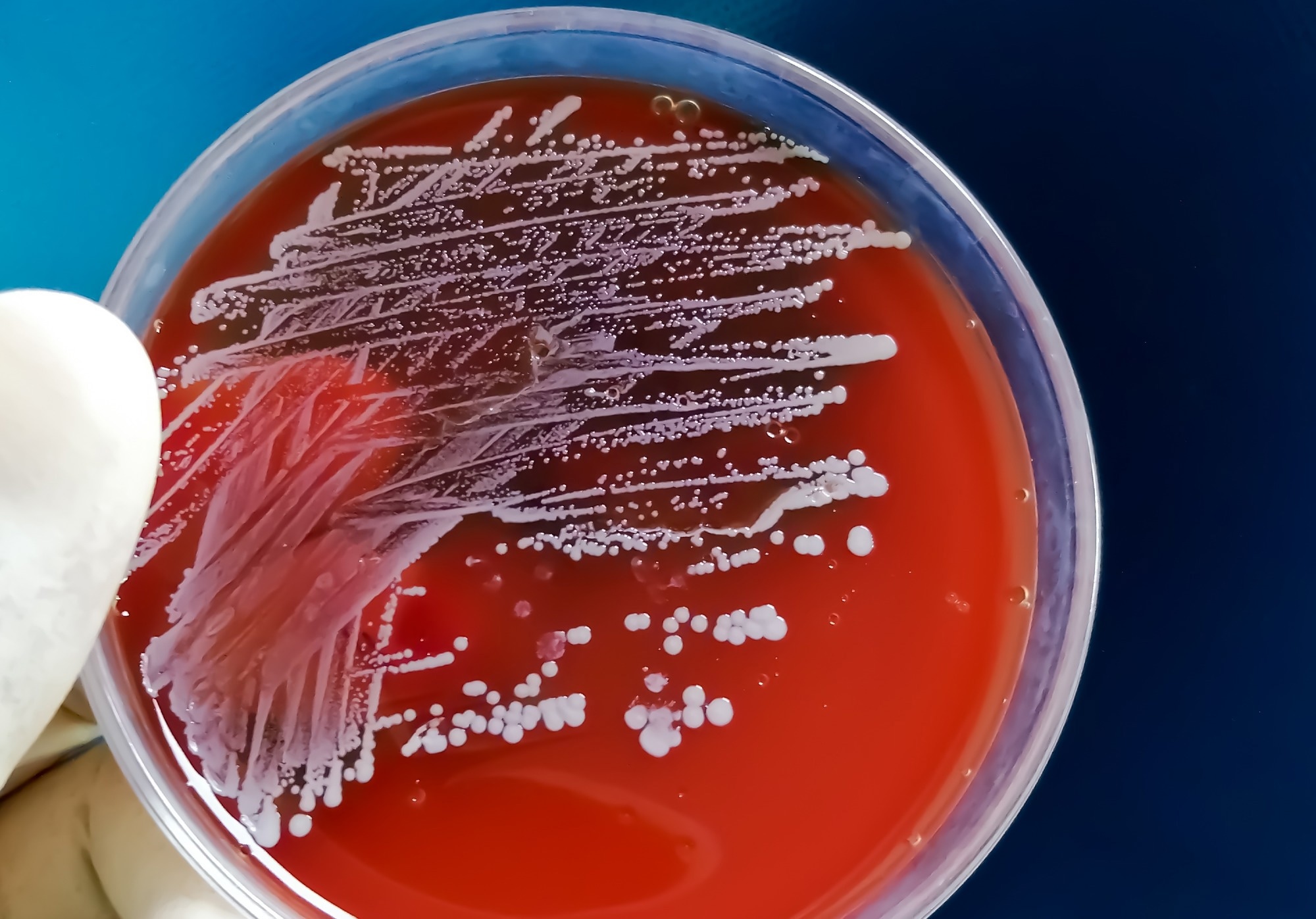 Image Credit: Saiful52/Shutterstock.com
Image Credit: Saiful52/Shutterstock.com
What makes S. aureus so dangerous?
The virulence of S. aureus lies in its ability to adapt to environmental pressures and immune defenses quickly. A central feature of its survival strategy is the accessory gene regulatory (Agr) two-component system (TCS), which helps control the production of key virulence factors.
When bacterial populations increase within host tissues, the Agr system is activated, triggering toxin production. As the infection progresses, Agr activity is downregulated, helping the bacteria evade immune detection.
Notably, some community-acquired MRSA (CA-MRSA) strains carry a dysfunctional Agr system, which is associated with more severe disease outcomes.2
Adhesion and invasion of host tissues
Colonization is the first step in S. aureus infection. It commonly inhabits the nostrils and skin, with about 15% of the population being persistent carriers. The bacterium typically infects damaged skin.
One of its key toxins, α-toxin, compromises epithelial barriers by activating the metalloproteinase ADAM10, which disrupts cell junctions.1
To adhere to host tissues, S. aureus uses surface proteins from the MSCRAMM family - such as staphylococcal protein A (SpA), fibronectin-binding proteins (FnbpA/B), and clumping factors (ClfA/B) - which bind to components like collagen and fibrinogen.
These interactions not only facilitate colonization but also promote immune evasion by inducing clot formation or platelet aggregation.1
Toxins and enzymes: Tools for survival and spread
Once established, S. aureus produces an extensive range of toxins and enzymes that enable it to invade tissues, evade immune responses, and extract nutrients.
These include pore-forming toxins such as α-toxin and various leukocidins that damage host cell membranes. Hemolysins target red blood cells, while phenol-soluble modulins (PSMs), like PSMα, commonly found in CA-MRSA, contribute to inflammation and cytolysis of both red and white blood cells.3
The bacterium also secretes exoproteins, including nucleases, proteases, lipases, hyaluronidase, and collagenase, which break down host tissues into usable nutrients.1
Additional virulence factors include exfoliative toxins A and B (ETA and ETB), which disrupt skin integrity, and EDIN exotoxins, which facilitate tissue invasion.3
Enterotoxins such as SEA, SEB, and SECn, along with toxic shock syndrome toxin-1 (TSST-1), act as superantigens, triggering uncontrolled immune activation, high fevers, and potentially fatal systemic inflammation. Some of these enterotoxins can also contaminate food, leading to staphylococcal food poisoning.3
Immune evasion mechanisms
S. aureus excels at evading the immune system. It often escapes from the bloodstream into tissues, where it forms abscesses - dense bacterial clusters surrounded by immune cells that it effectively traps outside.1
It also invades both phagocytic and non-phagocytic cells, allowing it to persist within host tissues and avoid immune clearance.
The bacterium interferes with neutrophil function at multiple levels: it prevents their migration, suppresses their activation, and neutralizes their killing mechanisms.
Enzymes such as superoxide dismutase (SOD), staphyloxanthin, and SPIN protect the bacterium from reactive oxygen species, while nucleases break down neutrophil extracellular traps (NETs).1
Immune shielding is further enhanced by biofilm formation, protective capsules, and cloaking within fibrin clots. Surface protein A (SpA) plays a dual role by masking bacterial antigens and diverting antibody production toward itself, effectively distracting the immune system 1
Leukocidins, including Panton-Valentine leukocidin (PVL), are especially dangerous, as they destroy white blood cells even at low concentrations. All S. aureus strains produce these cytolytic toxins and contribute significantly to tissue damage and immune suppression.
Beyond antibody evasion, S. aureus also induces anti-inflammatory responses and adaptive immune tolerance, further complicating the host’s ability to eliminate the infection.1
Clinical impact
S. aureus is responsible for a broad spectrum of diseases. These include skin infections like boils, abscesses, and impetigo, as well as more serious conditions such as pneumonia, surgical site infections, osteomyelitis, bacteremia, sepsis, and infective endocarditis.2
Biofilm-producing strains are particularly problematic for patients with prosthetic devices or implants.2
The bacterium’s exfoliative toxins cause dramatic conditions such as staphylococcal scalded skin syndrome (SSSS) and bullous impetigo, which involve extensive skin peeling and vulnerability to secondary infections.1
In the U.S. alone, S. aureus bacteremia leads to an estimated 20,000 deaths annually - more than AIDS, tuberculosis, and hepatitis combined.2
Antibiotic resistance: The rise of MRSA
One of the most alarming traits of S. aureus is its ability to develop antibiotic resistance rapidly. Methicillin-resistant S. aureus (MRSA) strains acquire resistance through mobile genetic elements (MGEs), making them difficult to treat.2 MRSA now accounts for over 50% of S. aureus infections in hospitalized patients.
While hospital-acquired MRSA (HA-MRSA) is well-known, community-acquired MRSA (CA-MRSA) has emerged as an even more aggressive variant. Its smaller MGE enhances both its virulence and its transmission potential.2
References
- Cheung, G. Y. C., Bae, J. S., and Otto, M. (2021). Pathogenicity and virulence of Staphylococcus aureus. Virulence. doi: https://doi.org/10.1080/21505594.2021.1878688. Available at https://pmc.ncbi.nlm.nih.gov/articles/PMC7872022. Accessed on February 11, 2025.
- Yamazaki, Y., Ito, T., Tamai, M., et al. (2024). The role of Staphylococcus aureus quorum sensing in cutaneous and systemic infections. Inflammation and Regeneration. doi: https://doi.org/10.1186/s41232-024-00323-8. Available at https://inflammregen.biomedcentral.com/articles/10.1186/s41232-024-00323-8. Accessed on February 11, 2025.
- Ahmad-Mansour, N., Loubet, P., Pouget, C. et al. (2021). Staphylococcus aureus Toxins: An Update on Their Pathogenic Properties and Potential Treatments. Toxins. doi: https://doi.org/10.3390/toxins13100677. Available at https://www.mdpi.com/2072-6651/13/10/677. Accessed on February 11, 2025.
Further Reading
Last Updated: Apr 18, 2025