The study was led by the Public Health Informatics, Computational, and Operations Research (PHICOR) team at the City University of New York (CUNY) Graduate School of Public Health and Health Policy (CUNY SPH) along with the Infectious Disease Clinical Outcomes Research Unit (ID-CORE) at the Los Angeles Biomedical Research Institute, Harbor-UCLA Medical Center and Torrance Memorial Medical Center.
The statistics come from a computer simulation model developed by the team to reflect what would probably happen in the entire country if various percentages of the population were to acquire the SARS-CoV-2. The simulation model shows the possible course of events following the spread of the infection.
The program also estimates the healthcare expenses incurred by Infected individuals. Each person infected would develop different symptoms as time passes. Thus, over time, such persons will make use of different segments of the healthcare system, including clinics, emergency departments, or hospitals.
At each stage, the patients will need health care providers, medications, hospital beds, and ventilators, based on how sick they become. These are factored in to calculate the costs involved, the resources needed, and the outcomes each patient can expect.
Once all this is put in place, the simulation tracks the financial and resource costs, as well as the outcomes.
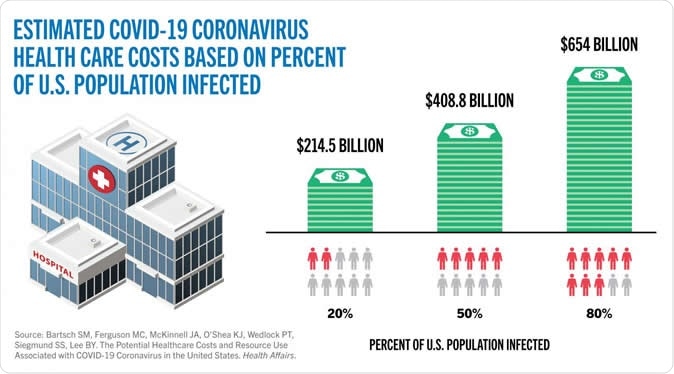
Estimated COVID-19 coronavirus health care costs based on percent of US population infected. Image Credit: CUNY SPH / Shutterstock
Tracking costs at increasing infection rates
The results showed that if only 20 percent of the U.S population were to be infected, hospitalizations would average 11.2 million, and patients would require approximately 1.6 million ventilators. The direct medical costs for this scenario averaged $163.4 billion for the duration of the infection.
The researchers also describe the factors that could result in 13.4 million hospitalizations, and the need for 2.3 million ventilators, pushing direct medical costs up to around $214.5 billion.
This was concerning, considering that there are only approximately 96,596 ICU beds and 62,000 ventilators in the U.S currently, as estimated by the Society of Critical Care Medicine. "Of course, the actual capacity used will depend on the timing of when patients need them," said Bartsch.
The study went on to simulate what would happen if half the population got infected - 27.9 million hospitalizations, 4.1 million ventilators, and 156.2 million hospital days, which might cost an average of $408.8 billion in direct medical costs.
If 80 percent were to get infected, the healthcare system would see 44.6 million hospitalizations, 6.5 million ventilators, and 249.5 million hospital bed days (which includes both general ward plus ICU bed days) costing a staggering $654 billion.
Letting the epidemic run its course
The study has enormous implications for policymakers, pointing out the difference in medical costs for various strategies employed that are directed at reducing infections, and the economic cost of letting the virus run its course.
In particular, "herd immunity" strategies have been advocated by some. Herd immunity consists of allowing the virus to spread until most of the population has been infected. These presumably immune people now act as a natural shield against the further spread of the virus to the uninfected people. However, in this study, lead author Sarah Bartsch warns this may deal significant damage to the economy. She says, "Such strategies could come at a tremendous cost."
As leaders mull over the possibilities of "re-opening" the country, senior author Bruce Y. Lee warns this is another recipe for disaster. If economic activity is allowed, and social distancing is relaxed, while the virus is still circulating, Lee warns that infections will surge with inevitable accompanying dramatic increases in healthcare spending.
"Such costs will affect the economy as well because someone will have to pay for them. Any economic argument for re-opening the country needs to factor in health care costs," he added.
Not exactly "just like the flu"
For others arguing that COVID-19 is "just like the flu," the study has cost comparisons - a single COVID-19 patient with symptoms accounts for $3,045 in direct medical costs just while he/she is infected, not counting costs if there are long-term effects of the infection. This is four times higher than the costs for treating a person with symptoms of influenza and 5.5 times higher than a person with symptoms of whooping cough.
"This is more evidence that the COVID-19 coronavirus is very different from the flu," said Bartsch. "The burden on the health care system and the resources needed are very different."
The study also factored in costs incurred by patients suffering from long-term effects of the illness. Though researchers are still assessing their nature, a small percentage may suffer continuing effects of the illness, including lung scarring and fibrosis. If long-term effects were considered, the average direct medical cost for a single patient rises to $3,994.
"Factoring in the costs incurred after the infection is over also adds to the costs. It is important to remember that for a proportion of the people who get infected, health care costs don't end when the active infection ends," Lee warned. "This pandemic will have its lasting effects, and taking care of those who will suffer continuing problems is one of them."
Preparing for shortages in healthcare
The model adds to the concerns of healthcare professionals and public health officials, who are already facing hospital bed and ventilator shortages as cases continue to rise. Bartsch describes the gap in the need and the availability of healthcare resources – people, machines, and beds – as being in "orders of magnitude."
Hopefully, this and similar studies will help make wise decisions about opening up the economy and preparing a greater health system capacity, by quantifying in greater detail the healthcare needs that may arise at various phases of the pandemic, especially with a rise in the percentage of people infected.
Source:
Journal reference:
- The Potential Health Care Costs And Resource Use Associated With COVID-19 In The United States Sarah M. Bartsch, Marie C. Ferguson, James A. McKinnell, Kelly J. O’Shea, Patrick T. Wedlock, Sheryl S. Siegmund, and Bruce Y. Lee Health Affairs, https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.00426