The ongoing COVID-19 pandemic has caused nearly five million cases and over 327,000 deaths worldwide. The signs and symptoms of this disease are varied, although there are typical features which assist diagnosis.
In Madrid, Spain, there have been over 66,000 reported cases, with over 40,000 hospital admissions until the first week of May. In most cases, symptoms are mild or nil. Another smaller set of patients manifests moderate sickness, while about 5 percent develop life-threatening complications, apparently due to an overactive immune response.
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (green) heavily infected with SARS-COV-2 virus particles (purple), isolated from a patient sample. Image captured and color-enhanced at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Reason for exploring links between COVID-19 and rheumatic disease
Researchers have noted that COVID-19 has a higher case rate and severity in patients who have risk factors like being older or having underlying medical conditions such as hypertension, diabetes, heart disease, and prior history of lung disease. The effect of a history of rheumatic disease on the risk for COVID-19 is not apparent, neither is it known if this predisposes COVID-19 patients to the risk of more severe infection or a worse outcome. This is not the case with previous outbreaks of coronavirus-caused respiratory illnesses such as SARS or MERS.
Early studies on COVID-19 patients show that the presence of chronic rheumatic conditions or treatment with disease-modifying anti-rheumatic drugs (DMARDs) do not confer increased risk for respiratory or fatal complications as compared to the general risk.
Now, a new study published on the preprint server medRxiv* explores the risk factors for hospital admission in patients with inflammatory rheumatic diseases (IRD) and COVID-19.
How was the IRD-COVID-19 risk factor study carried out?
The study was carried out from March 1, 2020, to April 24, 2020, at a tertiary hospital in Madrid. All patients who attended the rheumatology outpatient clinic during this period were enrolled in the study, if they were over 16 years of age, were diagnosed with IRD, and had symptomatic COVID-19, either by clinical criteria or by the reverse transcription-polymerase chain reaction (RT-PCR) test.
The data collected from these patients included sociodemographic characteristics, the type of inflammatory rheumatic disease, and the incidence of other diseases at baseline, such as lung or liver disease, diabetes, hypertension, smoking, kidney disease, and hyperlipidemias. Thyroid, heart and vascular disease were also noted. The researchers also included any treatment for IRD and the type, if so. Disease-modifying anti-rheumatic drugs (DMARDs) had to begin a month or more before the study, continue through March 21 or longer, or until admission or the end of the study.
The hospital admissions were reviewed to make sure that all were related to COVID-19 rather than other conditions.
There were 123 IRD patients with symptoms of COVID-19, mostly women aged 60 years, on average, with the disease having evolved over 10.7 years on average. The primary diagnosis was rheumatoid arthritis, in 41%, followed by axial spondyloarthritis in 15% of patients. Many patients also had one or more additional conditions, mostly high blood pressure, high blood cholesterol, and lung disease.
Most patients were on conventional synthetic DMARDs at the start of the study, half on glucocorticoids and a quarter on nonsteroidal anti-inflammatory drugs (NSAIDs). A fifth was on biologic DMARDs, with 6.5% on Adalimumab and 4% on Rituximab. About 15% of patients on biologics were also on synthetic DMARDs.
Among these 123 patients, 54 needed hospitalization due to COVID-19. About 60% were women, and the mean age was 70 years, with the median duration from the first symptom to admission being five days. The duration of stay was a median of 9 days.
Most patients (86%) were put on hydroxychloroquine, and 52% were treated with corticosteroids. Another 18 were on antivirals and 3 on the anti-IL-6 drug tocilizumab.
About 20 patients developed complications while in hospital, most commonly myocarditis, thrombosis, and kidney failure. Only 2 required intensive care unit (ICU) admission.
What did the researchers conclude?
The analysis showed that being elderly, as well as having any of the following medical conditions, increased the risk of hospital admission: chronic inflammatory arthritis, hypertension, diabetes, heart disease, and lung disease. The use of NSAIDs or biologics targeting TNF had a smaller association. Glucocorticoids tended to increase the risk, while antimalarials lowered the risk.
Multivariate analysis failed to confirm a statistical difference between different types of DMARDs. The only risk factors were older age and the presence of systemic autoimmune conditions. Glucocorticoids, any of the diseases listed below, and the female sex, also showed a trend towards higher risk for admission. However, this was not statistically significant - diabetes mellitus, pulmonary disease, ischemic vascular disease, hypertension, venous thrombosis/lung embolism, lung disease, and or liver disease.
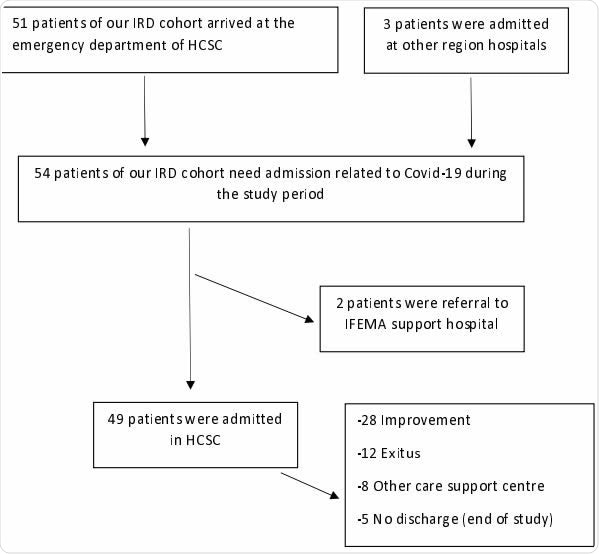
Flow chart for COVID-19 patient hospital admission
The median age among admitted patients was a good 15 years older than that of non-admitted patients, while that of fatalities was over 80 years. This is in keeping with the mortality trend in the general population, where over half of all deaths were in the age group of 80 or older, and 95% in those over 60 years.
Diabetes was found to be an independent risk factor for COVID-19, admission to the ICU, and death due to this disease. The higher the number of coexisting medical conditions, the worse the clinical outcome, beginning from single comorbidity.
The study shows that about 44% of patients with IRD and COVID-19 will need hospital admission, most of this subgroup being elderly patients with other medical conditions and systemic autoimmune disease. However, it supports earlier evidence that DMARDs do not increase the risk of hospital admission for COVID-19 related symptoms and signs.
Females did not have a higher risk for admission despite being at an increased risk for rheumatic disease. Systemic autoimmune diseases were associated with the highest risk of admission.
The observational nature of the study, and the recording of data in a standard heavy workload environment, makes it likely that much of the information was incomplete. Many patients may have been lost for follow up in the non-hospitalized group. About a fifth of cases did not have the diagnosis confirmed by RT-PCR.
Also, ethnic diversity in relation to the difference in the severity of COVID-19 was not studied. Nonetheless, the study identifies some possible risk factors that may help inform patients with IRD about minimizing risk and predicting increased risk for hospitalization among these patients.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Freites, D. et al. (2020). Risk Factors for Hospital Admission Related To COVID-19 In Inflammatory Rheumatic Diseases. medRxiv preprint. doi: https://doi.org/10.1101/2020.05.14.20101584.
- Peer reviewed and published scientific report.
Nuñez, Dalifer D. Freites, Leticia Leon, Arkaitz Mucientes, Luis Rodriguez-Rodriguez, Judit Font Urgelles, Alfredo Madrid García, Jose I. Colomer, Juan A. Jover, Benjamín Fernandez-Gutierrez, and Lydia Abasolo. 2020. “Risk Factors for Hospital Admissions Related to COVID-19 in Patients with Autoimmune Inflammatory Rheumatic Diseases.” Annals of the Rheumatic Diseases 79 (11): 1393–99. https://doi.org/10.1136/annrheumdis-2020-217984. https://ard.bmj.com/content/79/11/1393.