The COVID-19 pandemic is still extremely active in many parts of the world, having caused millions of cases in just five months. Several subgroups are at high risk of severe or even fatal disease. Now, a new study published in June 2020 on the preprint online server medRxiv* reports on the increased risk of COVID-19 in Down Syndrome (DS) and certain characteristic features that are found in this population segment.
Down syndrome describes trisomy 21, a condition in which the individual has three copies of the 21st chromosome instead of two. It is present at birth, and there are about 250,000 affected individuals in the world at present. The impact of COVID-19 on DS individuals is unknown. However, they are known to have a higher risk of respiratory tract infections, including and especially caused by influenza and respiratory syncytial viruses.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The current study aims at identifying the risk of this infection in people what have DS. In this retrospective study, the researchers examined the medical records of over 4,600 people admitted to Mount Sinai hospitals with COVID-19 from March 1 to April 24, 2020.
All patients had their diagnosis confirmed by RT-PCR. In this retrospective study, DS patients were identified from their electronic medical records. For each such individual, six random controls were chosen with matching age, race, and sex characteristics.
The researchers also retrieved demographic information, vital signs, laboratory readings, and outcome data from the records.
Judging from the 2.6 million patient inflow to this hospital system over the last five years, with about 1,100 DS patients, the expected number of COVID-19 patients with DS was 2. However, when the age composition of patients with DS is accounted for, the number of expected DS is nearer 1.
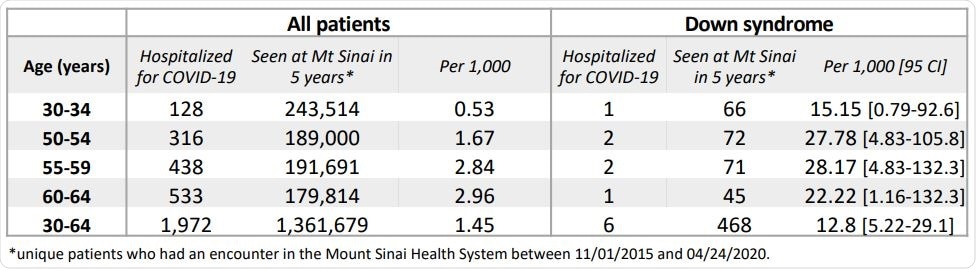
Estimated COVID-19 hospitalization rates in the Mount Sinai Health System in DS and non-DS patients.
The current study showed that 6 DS patients were admitted with COVID-19, which is far above the expected number. This corresponds to a 9-fold increase in the percentage of hospitalized COVID-19 DS patients compared to that in the general population in the age group 30-64 years.
The median age of DS patients with COVID-19 who were in hospital was 54 years, which is more than 12 years younger than other COVID-19 patients at the same hospital. This suggests that DS patients are at an increased risk of hospitalization with COVID-19 from about ten years earlier than the general population.
Next, the investigators examined the DS-COVID-19 hospitalized patients in comparison with a larger (fivefold) control group matched for sex, race, and age with each patient. The control group had other existing conditions such as hypertension in about 13%, diabetes in about 10%, and obesity in 7%.
This was quite different in the DS group, which had hypothyroidism in about 67%, type 2 diabetes in about 50%, epilepsy in 50%, and dementia in 33%. This was in keeping with the high frequency of these conditions (except for type 2 diabetes) in people with DS.
The incidence of type I diabetes in DS is 3-4 times higher than in the general population. Diabetes is a known risk factor for severe COVID-19. Hypothyroidism in this subgroup is well controlled and is therefore unlikely to be a reason for COVID-19 disease. Neurological disease also boosts the odds of dying from COVID-19, according to one study, though the mechanisms are unknown.
The researchers summarized these findings, “Based on our data and previous findings, we conclude that patients with DS are not only more likely to be hospitalized with COVID-19, but also that their comorbid conditions, including diabetes, in particular, are important drivers.”
The study also looked at the levels of various inflammatory molecules and indicators such as the temperature, the C-reactive protein (CRP), ESR, and IL-8. The researchers failed to find significant differences between patients and controls in these, nor in the cell counts. There was a higher variance of IL-1b and IL-6, meaning that some DS patients have a hyperinflammatory response. This needs to be confirmed by further studies.
Finally, DS patients with severe COVID-19 had higher odds of developing complications of the disease, including acute respiratory distress syndrome (ARDS), acute kidney injury, and neurological symptoms. Sepsis was particularly common, with 4/6 DS COVID-19 patients developing sepsis compared to only 6/30 controls.
DS children who develop sepsis have a gloomier prognosis compared to other children with DS. This is, therefore, a condition that requires meticulous care, prevention of COVID-19, and early management. DS patients hospitalized with COVID-19 are at a higher risk of mechanical ventilation and requiring ICU admission, but the difference was not significant.
DS patients had a more extended hospital stay with a median of 17 days compared to non-DS controls at 8 days. A third of DS patients died vs. 7% of controls. This suggests that DS individuals with COVID-19 were at high risk of infection at an earlier age, though at this age, they are still above the 85th percentile for this population. Old age is a known risk factor for COVID-19.
DS individuals were significantly more likely to develop complications and to stay almost twice as long in hospital compared to non-DS controls. They were also at a much higher risk of dying from the infection. Diabetes is probably the most prominent risk factor for poor prognosis in DS patients.
Other immune factors that could play a role in DS-associated susceptibility to COVID-19 have not been well-studied so far. However, it is clear that sepsis is a widespread complication in the DS-COVID-19 cohort. This is important since these patients are more likely to die of sepsis than other septic patients.
The study warns, “Particular attention should be paid to both the prevention and treatment of COVID-19 in individuals with DS, as they are at higher risk of hospitalization induced complications during the SARS-CoV-2 pandemic.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Malle, L. et al. (2020). COVID-19 Hospitalization is More Frequent and Severe in Down Syndrome and Affects Patients a Decade Younger. medRxiv preprint. doi: https://doi.org/10.1101/2020.05.26.20112748. https://www.medrxiv.org/content/10.1101/2020.05.26.20112748v1
- Peer reviewed and published scientific report.
Malle, Louise, Cynthia Gao, Chin Hur, Han Q. Truong, Nicole M. Bouvier, Bethany Percha, Xiao-Fei Kong, and Dusan Bogunovic. 2020. “Individuals with down Syndrome Hospitalized with COVID-19 Have More Severe Disease.” Genetics in Medicine, October. https://doi.org/10.1038/s41436-020-01004-w. https://www.gimjournal.org/article/S1098-3600(21)04944-3/fulltext.