The ongoing coronavirus disease 19 (COVID-19) pandemic has claimed over 1.2 million lives worldwide and impacted economies in unprecedented ways. Although many COVID-19 patients survive the illness, there are increasing numbers of patients who are "cleared" of the virus but still experience symptoms and require hospitalization.
The hospitalization and re-admission of COVID-19 patients after viral clearance has been a topic of significant interest in minimizing mortality as well as healthcare costs. Previous studies focused on hospitalization and re-admission post recovery from other illnesses like influenza, heart failure, and pneumonia have concluded that most re-admissions resulted from complex interactions between the host's recovering immune system and the inflammatory response. Minimal data is currently available on the long-term effects of COVID-19 in those who are cleared of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
The current gold standard for determining the clearance of SARS-CoV-2 from patients recovering from COVID-19 is two consecutive negative results in a real-time reverse transcription-polymerase chain reaction (RT-PCR) test. Patients requiring hospitalization due to protracted COVID-19 complications, despite confirmed viral clearance, present a clinical conundrum.
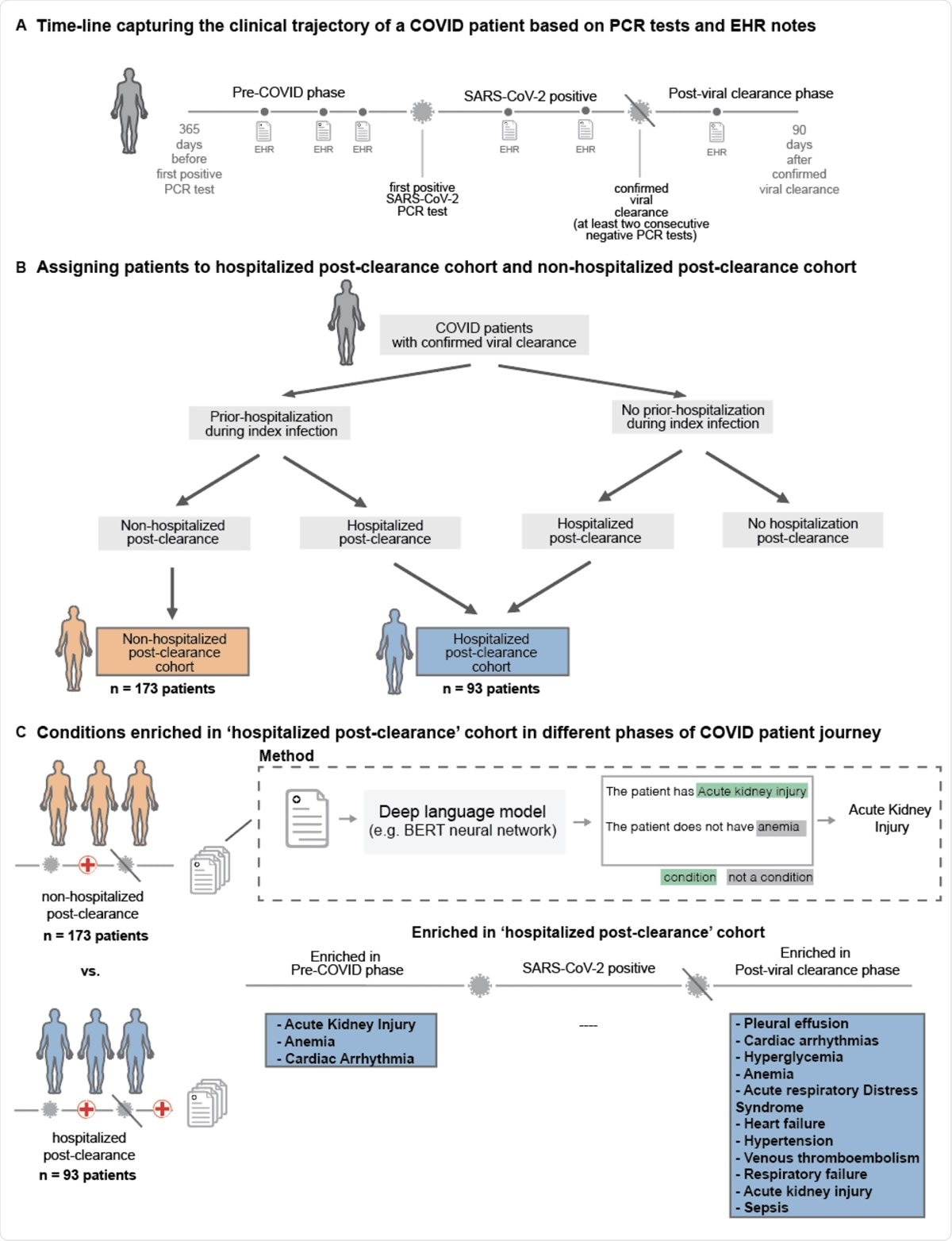
Overall study design. (A) Trajectory of a COVID-19 patient transitioning from pre-COVID (time up to 365 days before first positive PCR test) through the SARS-CoV-2 positive phase (interval after first positive test but before the first of two consecutive negative PCR test results) into the post viral clearance phase (period up to 90 days after the first of two negative PCR test results), (B) Demonstrates procedure for assigning patients to the hospitalized post-clearance cohort and non-hospitalized post-clearance cohort patients can be hospitalized at varying points in time including during the index infection (time from first positive PCR test results to first of two negative PCR test results) and following viral clearance - two cohorts are defined from the overall population, Hospitalized Post-Clearance Cohort in which patients are admitted or readmitted to the hospital following their estimated clearance date and Non-Hospitalized Post-Clearance Cohort in which patients are admitted during the index infection, but not following the estimated clearance date, (C) For each patient if the two defined cohorts a deep language (BERT) model is used to extracted phenotypes of interest from the clinical notes recorded between 365 days prior to infection and up to 90 days after clearance for each patient - occurrences of these phenotypes are stratified into pre-COVID, COVID pre-clearance, and COVID post-clearance time periods and statistical tests are run to find significant differences in phenotypes between the two cohorts.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Using retrospective analysis to study patients re-admitted after viral clearance
Researchers from the nference (a biotech information firm) in Cambridge, MA, USA, the Mayo Clinic in Rochester, MN, USA, and nference Labs based in Bengaluru, India, recently performed a retrospective analysis of 266 COVID-19 patients. This analysis compared those admitted or re-admitted after viral clearance with those who were hospitalized before viral clearance but did not require hospitalization after viral clearance. Their study has been published on the preprint server, medRxiv*.
To differentiate these two study cohorts, they used neural network models to curate comorbidities and complications from the physician notes in these patients' health records. The physician notes of the hospitalized post-viral clearance group showed acute kidney injury (n=15 (16.1%)), anemia (n=20 (21.5%)), and cardiac arrhythmia (n=21 (22.6%)) in the year preceding the onset of COVID-19.
Preexisting health conditions increase the risk of post-COVID hospitalization
This is the first study carried out at a major healthcare center that analyzes the risk factors behind post-viral clearance hospitalization in some COVID-19 patients. This study used augmented curation to gather complications and comorbidities from patients' health records instead of relying on the international classification of diseases (ICD) codes for data. The statistical analysis performed in this study identified comorbidities that existed a year before confirmed diagnosis of SARS-CoV-2 infection by PCR testing. Preexisting conditions were associated with higher rates of hospitalization post-viral clearance.
The results of this study showed that preexisting conditions play a key role in hospitalization risk in COVID-19 patients after confirmed SARS-CoV-2 viral clearance. Their findings say that pre-COVID anemia increases the risk of post-COVID hospitalization, which is concerning because of the endemic nature and high prevalence of anemia in many under-developed and developing countries, which are currently seeing a huge number of COVID-19 cases and related mortality.
"Finally, this study also emphasizes the need for detailed curation of structured and unstructured clinical data to better understand the dynamics of viral clearance, underlying conditions, and long-term complications."
Findings highlight the need for follow-up research into specific risk factors for post-COVID hospitalization
The authors believe that their study will motivate further follow-up research into specific risk factors they have identified that seem to predispose some patients with preexisting conditions to long-lasting adverse effects of COVID-19. They hope that their findings of possible long-term effects of SARS-CoV-2 infection inspire more studies that will help find effective prophylactic and therapeutic interventions to treat COVID-19.
"Overall, our finding of the long-term adverse effects of COVID-19 motivates the need to understand the biological and mechanistic underpinning of the SARS-CoV-2 driven long-term adverse effects in order to find appropriate prophylactic and therapeutic interventions."
The authors also discuss some limitations of their study. The dataset used by this study is from a single healthcare system, so the clinical characteristics of the study cohort may be biased and may reflect clinical characteristics of individuals receiving treatment in some regions of the USA such as Arizona, Florida, or Minnesota. They also use the first of two consecutive negative PCR test results to measure viral clearance for each patient, but the actual viral clearance date is unknown.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Pawlowski, C. et al. (2020) Preexisting conditions are associated with COVID patients' hospitalization, despite confirmed clearance of SARS-CoV-2 virus; https://doi.org/10.1101/2020.10.28.20221655, https://www.medrxiv.org/content/10.1101/2020.10.28.20221655v2
- Peer reviewed and published scientific report.
Pawlowski, Colin, AJ Venkatakrishnan, Eshwan Ramudu, Christian Kirkup, Arjun Puranik, Nikhil Kayal, Gabriela Berner, et al. 2021. “Pre-Existing Conditions Are Associated with COVID-19 Patients’ Hospitalization, despite Confirmed Clearance of SARS-CoV-2 Virus.” EClinicalMedicine 34 (April): 100793. https://doi.org/10.1016/j.eclinm.2021.100793. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00073-0/fulltext.