The findings indicate the need to build trust by engaging and trustworthy public communication from physicians, healthcare authorities, and scientists to foster a positive attitude to the vaccine.
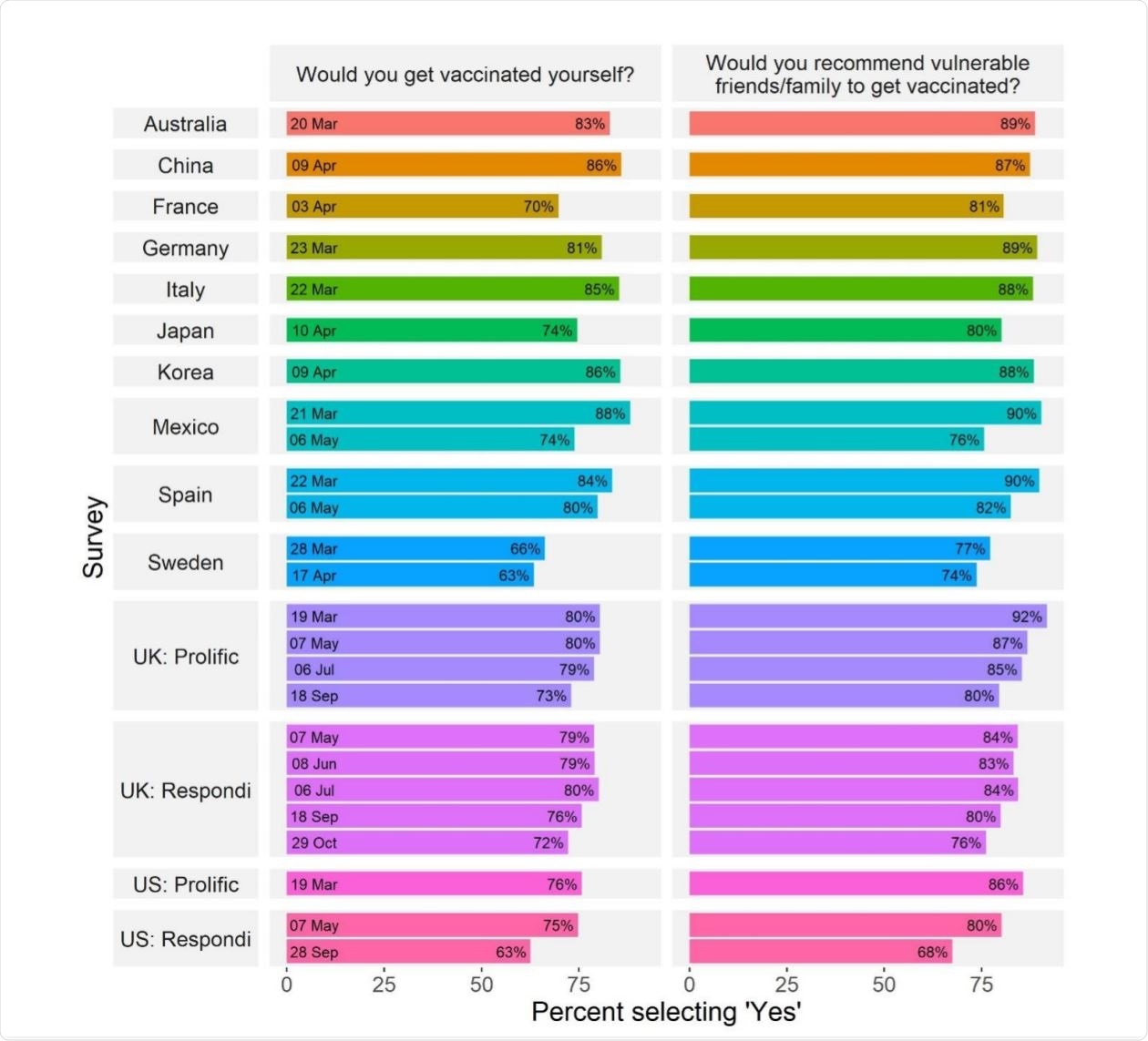
COVID-19 vaccine acceptance across countries and time. Image Credit: https://www.medrxiv.org/content/10.1101/2020.12.09.20246439v1.full.pdf

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Importance of Vaccination
Even as the world crosses the dismal milestone of more than 1.6 million COVID-19-related deaths, it is evident that herd immunity is still far off. Vaccination will be necessary to achieve a level of population immunity that will prevent spread.
Apart from the technological challenges of getting a vaccine ready, one of the biggest obstacles in reaching this goal is vaccine hesitancy, that is, a delay in accepting a vaccine when available or refusing it altogether.
This could lead to the unnecessary prolongation of the pandemic even after a vaccine is rolled out and additional losses among the susceptible population, including people who cannot be vaccinated for legitimate reasons. According to the World Health Organization (WHO), vaccine hesitancy is among the top 10 threats to health on a global scale.
Earlier Findings on Vaccine Hesitancy
While much research has already taken place with respect to the risk factors for vaccine hesitancy, there is a difference where COVID-19 vaccines are concerned. There is a lack of firm information, while uncertainty and misinformation are at an all-time high. Trust in scientific institutions and governmental authorities has also eroded considerably.
Several studies show that older people, those who show more trust in the government, and men, are more likely to accept the vaccine worldwide. The current study aims to elucidate the precise nature of this lack of trust: is it aimed at governments, hospitals, scientists, other people, or some or all of these entities? Secondly, is such mistrust general or only focused on their actions and attitudes to COVID-19?
Risk perception is another crucial factor in deciding vaccine attitudes. Political biases and elitist perceptions can also play a significant role in accelerating anti-vaccination attitudes.
Study Details
To put all these together, the current study looks at significant social, political, and psychological risk predictors of public attitudes towards COVID-19 vaccines.
Carried out across 12 countries, with some countries having had more than one survey, the study covers over 25,000 participants.
Prominent Risk Factors
All the samples showed that between ~63% and 88% of respondents said they were willing to get the vaccine shot. Interestingly, between 68% to 91% said they would advise vulnerable people to be vaccinated. This gap was observed to be consistent in every single sample.
Secondly, vaccine hesitancy decreased over time in almost every case where more than one survey was taken in the same country. For instance, it fell by 12 and 15 points in the US and Mexico, respectively.
The level of vaccine acceptance was higher by 27% in individuals who said they trusted experts to know the best measures to take about the pandemic, but by almost 50% among people with higher risk perception. Males were more likely to get the vaccine, at 41% higher rates than women. There was no observable difference in measures of efficacy and reported vaccine acceptance.
One interesting finding of the study was the significant variation in the type and contribution of different risk factors to vaccine hesitancy. For example, in the US, conservatives had 27% lower odds of accepting the vaccine, while having trust in expert recommendations and heightened personal risk perception boosted the chances of getting the vaccine by 53% (38% at the later survey, in May), and 48% (down to 27% by May), respectively.
However, in the UK, age, sex, and social biases played a significant role in deciding vaccine acceptance, though this also changed over time. Conservative political views tended to have 16% lower vaccination intentions from September 2020, perhaps due to more substantial splits between different viewpoints.
Overall, the important variables driving vaccine hesitancy in the UK were the individual’s sex, age, risk perception about the virus, and the level of trust in WHO-backed COVID-19 recommendations, trust in national scientific advisors and politicians regarding the COVID-19, as well as trust in general.
What are the Implications?
Interestingly, the UK showed a variation in the vaccine acceptance profile when samples from different survey providers were used, even when the collectors obtained the same data. This difference persisted even after adjusting for age, sex, and other demographics. This shows the importance of using multiple samples rather than generalizing from one sample.
The different factors explored in this study explained about 10% to 30% of the total difference between vaccine acceptors and others, but the percentage of variance explained was lower with Japan and Korea, at 8% and 4%, respectively. The researchers found that even when adjusted for general attitudes towards vaccination, the results remained largely unchanged.
In general, negative attitudes towards vaccination did predict negative attitudes towards COVID-19 vaccine refusal significantly. However, the current vaccine is different, chiefly because of its accelerated development and shortened trial periods. This has raised the specter of potentially overlooked safety issues, particularly in the long term.
There is no apparent reason for the male orientation towards vaccine acceptance relative to female. The attitude towards the vaccine also appears to be increasingly politicized, a fait accompli in the US and well on the way in the UK.
a pattern of attitudinal alignment over time in a small UK sample, resulting in the emergence of a politically conservative faction expressing less trust in scientists, doctors, and vaccines.”
Whether this is the case outside the US and the UK will require further studies, as this data is not available. However, there is a high possibility that pandemic-related misinformation and conspiracy theories, rampant among those with right-wing affiliations, have made a significant contribution to this state of affairs.
Conclusions
The researchers say, “The bulk of the burden of trust rests on science and medicine. Trust in government and general social trust are not significantly associated with vaccine acceptance in most of our samples.”
Another beneficial contributor may be prosociality, where it may be useful to emphasize that receiving the vaccine helps protect others who are vulnerable, rather than the vaccinees directly, who may not perceive themselves as being at any particular risk.
Our finding highlights the need to work proactively with others from outside of this sphere, such as community and religious leaders to open a two-way conversation with those who distrust the scientific and medical establishment.”
This demands research on the best way to communicate the truth about the vaccine in a medium that is accessible and acceptable. Care should also be taken to address genuine and deep concerns regarding this vaccine.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Kerr, J. R. et al. (2020). Predictors of COVID-19 vaccine acceptance across time and countries. medRxiv preprint. doi: https://doi.org/10.1101/2020.12.09.20246439. https://www.medrxiv.org/content/10.1101/2020.12.09.20246439v1
- Peer reviewed and published scientific report.
Kerr, John R., Claudia R. Schneider, Gabriel Recchia, Sarah Dryhurst, Ullrika Sahlin, Carole Dufouil, Pierre Arwidson, Alexandra LJ Freeman, and Sander van der Linden. 2021. “Correlates of Intended COVID-19 Vaccine Acceptance across Time and Countries: Results from a Series of Cross-Sectional Surveys.” BMJ Open 11 (8): e048025. https://doi.org/10.1136/bmjopen-2020-048025. https://bmjopen.bmj.com/content/11/8/e048025.