The current pandemic of novel coronavirus disease 2019 (COVID-19) was caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has undergone numerous mutations in its genome to emerge as different variants. As of now, a dozen vaccines have received emergency use authorization, and many countries around the world have initiated mass vaccination campaigns.
Variants of concern and spike mutations
Most vaccines now in use or being developed focus on generating antibodies to the viral spike protein, which mediates host cell entry and infection. This is based on the strong correlation between neutralizing antibodies to the spike and protective immunity.
The world has recently witnessed the emergence of highly transmissible and virulent variants of SARS-CoV-2, however. The current study examines the extent to which vaccine-elicited antibodies neutralize these variants.
The first of these variants of concern (VOCs) is the UK variant, also called B.1.1.7 (501Y.V1, VOC 202012/01), which rapidly increased in prevalence since its first detection in November 2020, to make up 97% of sequenced genomes by the end of January 2021.
It has multiple mutations in the spike gene, indicating it may have arisen in an immunocompromised person during chronic infection. Not only does it spread faster, but it is also likely to cause higher case fatality.
Two more variants emerged, one from South Africa and the other from Brazil, termed B.1.351 and P.1, respectively. These were found to escape from neutralization when incubated with antibodies generated in response to the first wave of the pandemic. The result was several documented reinfections.
All three variants have the N501Y mutation in the spike receptor-binding domain (RBD), accompanied by two others in the B.1.351 and P.1 viruses - K417N/T and E484K.
E484K is established to be associated with escape from convalescent sera and monoclonal antibodies, respectively. Therefore, as expected, both these lineages show immune escape from first wave convalescent sera and vaccine-elicited antibodies.
However, these two variants appear to be less transmissible since their detection in the US has not been followed by a significant increase in cases. On the other hand, the E484K mutation has been found to emerge in several other lineages, which are showing an increase in different countries the world over.
One is B.1.526 sub-lineage, which shows a more rapid increase in prevalence than the UK variant, and may reinfect patients who have recovered from the first wave virus, thus evading herd immunity. Another is the P.2 lineage which has a single E484K mutation in the RBD, and is showing rapid spread to Argentina and other South American countries, following its detection in Brazil.
Stabilized pre-fusion spike is more immunogenic
The vaccines with the highest efficacy use a stabilized form of the spike protein with two paired proline substitutions, locking it into the prefusion form. Others, which use the wildtype spike, may protect against severe disease but not against infection because of the lower levels of neutralizing antibodies.
This has been observed to be true of the Astra-Zeneca ChAdOx1 vaccine, based on an adenovirus vector. In South Africa, where 93% of infections are due to B.1.351, the vaccine failed to prevent mild-to-moderate COVID-19.
The Sputnik V or Gam-COVID-Vac vaccine is also based on the wild-type spike. Its interim Phase 3 trial results have been reported to show a vaccine efficacy of 92%, but this did not include the currently circulating variants nor any lineage containing E484K.
The use of this vaccine in several countries in South America and eastern Europe, besides Russia, mandates that its efficacy against the new resistant variants be tested, as they are being found more commonly in these regions.
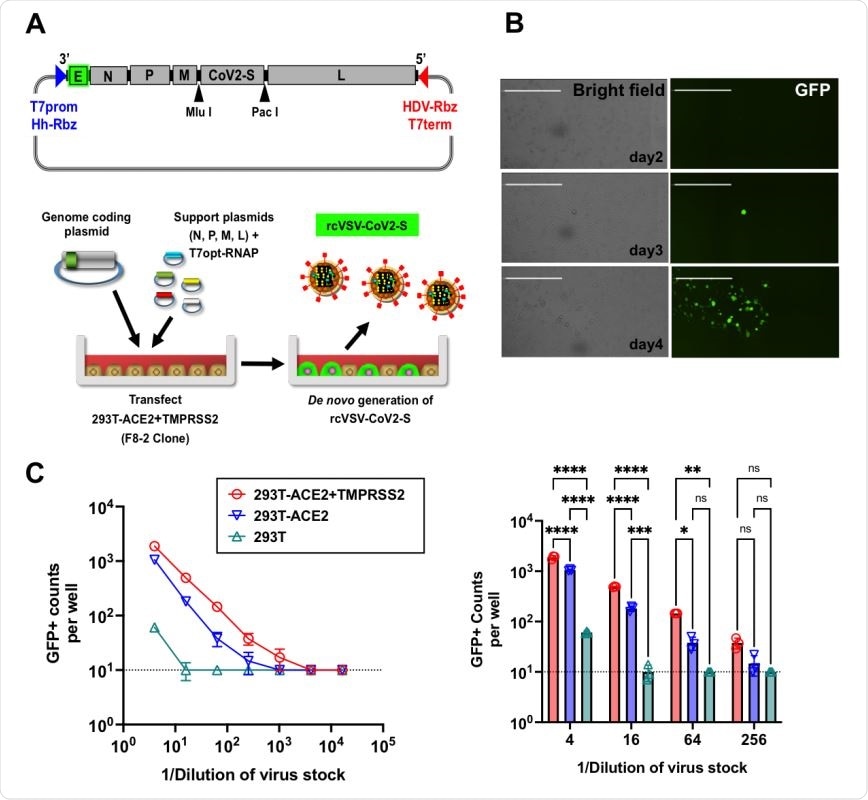
Generation of replication-competent VSV bearing SARS-CoV-2 spike (rcVSV-CoV2-S). (A) Schematic of the rcVSV-CoV2-S genomic coding construct and the virus rescue procedure. The maximal T7 promoter (T7prom) followed by a hammer-head ribozyme (HhRbz) and the HDV ribozyme (HDVRbz) plus T7 terminator (T7term) are positioned at the 3’ and 5’ ends of the viral cDNA, respectively. An EGFP(E) transcriptional unit is placed at the 3’ terminus to allow for high level transcription. SARS-CoV-2-S is cloned in place of VSV-G using the indicated restriction sites designed to facilitate easy exchange of spike variants or mutants. For virus rescue, highly permissive 293T-ACE2+TMPRSS2 (F8-2 clones) cells were transfected with the genome coding plasmid, helper plasmids encoding CMV-driven N, P, M, and L genes, and pCAGS encoding codon-optimized T7-RNA polymerase(T7opt-RNAP). 48-72 hpi, transfected cells turn EGFP+ and start forming syncytia. Supernatants containing rcVSV-CoV2-S are then amplified in Vero-TMPRSS2 cells. (B) Representative images of de novo generation of rcVSV-CoV2-S in transfected 293T-ACE2-TMPRSS2 (F8-2) cells as described in (A). Single GFP+ cells are detectable at 2-3 days post-transfection (dpt). Some of these form a foci of syncytia by 4 dpt. Images are taken by Celigo imaging cytometer (Nexcelom) and are computational composites from the identical number of fields in each well. White bar is equal to 1 millimeter. (C) Left panel: Entry efficiency of rcVSV-CoV2-S in parental 293T cells, 293T stably expressing ACE2 alone (293T-ACE2) or with TMPRSS2 (293T-ACE2+TMPRSS2). Serial dilutions of virus stocks amplified on Vero-TMPRSS2 cells were used to infect the indicated cell lines in 96-well plates in triplicates. GFP signal was detected and counted by a Celigo imaging cytometer (Nexcelom) 10 hpi. Symbols represent the average of 3 replicates with error bars indicating standard deviation. Right Panel: Data from the gray shaded box in the left panel is expanded to show the individual data points at the indicated dilutions. 2 way-ANOVA was used to compare the differences between cell lines at any given dilution. Adjusted p values from Tukey’s multiple comparisons test are given (ns; not significant, * p < 0.05, ** p < 0.01, *** p = 0.001, **** p < 0.001).

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
What were the study results?
The current study assays serum neutralization activity in samples obtained from a dozen Sputnik V vaccine recipients in Argentina. This country has already detected many independent E484K-bearing variants, with or without N501Y substitutions, in tandem with its vaccine rollout.
The researchers found that pseudoviruses bearing either the wildtype D614G spike, and the B.1.1.1.7 spike were effectively neutralized by the vaccine sera, in live virus plaque reduction neutralization assays. The geometric mean titer (GMT) of neutralizing titers was 49, similar to that of the phase III trial.
However, these sera showed moderate to a marked reduction in neutralization titers against spike protein bearing E484K, and the UK variant. Even at the highest serum concentration used, 9/12 serum samples were not capable of inhibiting 50% of B.1351 viral particles, and only half the sera did so against the E484K mutant.
The researchers concluded that virus neutralizing titers (VNTs) were reduced by seven- and three-fold against the B.1.351 lineage and E484K spike, respectively, relative to the wildtype spike.
Different modes
On further analysis, the neutralizing antibody response to the virus was classified into four. One group showed reasonably low 50% inhibitory concentrations (IC50) against wildtype and UK spike variants.
However, it could not reach IC90 even at the highest possible serum concentrations. Against E484K mutants, the IC50 is reduced, but neutralization will still occur at high serum concentrations.
The second group inhibits wildtype, B.1.1.7 and E484K spike at high concentrations but cannot inhibit the South African variant at the highest concentration.
The third group can neutralize both E484K and B.351 with similar IC50 to the wildtype and UK variants, more so at high serum concentrations.
The fourth group consists of one unusual serum with no neutralizing ability against the wildtype, E484K or B.1.351 variants, but with neutralizing capacity against the UK variant similar to the first group.
AstraZeneca vaccine serum results
This echoes the results obtained from AstraZeneca vaccine sera live virus plaque reduction neutralization assays, where the neutralizing activity against the South African variant B.1.351 dropped by 4- to 33-fold relative to the wildtype spike. Seven of 12 vaccine recipients whose sera neutralized the B.1.1 variant showed no neutralizing activity against B.1.351.
Similar, though smaller, reductions in neutralizing capacity were seen with the vaccine sera of Moderna/Pfizer vaccine recipients, at 7-8-fold.
Resistance to neutralization
When the vaccine was tested by assaying the inhibition of the wildtype and VOC spike proteins using soluble RBD-Fc, the spike-receptor affinity was found to follow classical dose-response curves. The Fc component of an antibody is the part that recognizes the receptor, in this case, the human angiotensin-converting enzyme 2 (ACE2).
Both the UK and the South African variant showed a slight decrease in RBD-Fc inhibition of viral entry, with a 1.5- and 2-fold rise in the IC50, respectively. This might have been expected from the fact that they both have the N501Y substitution associated with enhanced RBD-ACE2 affinity.
However, this is not consistent with the sensitivity of the UK variant spike in virus neutralization assays, as shown earlier. Thus, the findings suggest that the VOCs with these different spikes show different modes of escape from antibody-mediated neutralization by sera elicited by the Sputnik V vaccine.
In other words, the resistance to neutralization offered by the South African variant occurs by a different mechanism than that of the E484K mutant.
What are the implications?
This is the earliest study showing that the recipients of the Sputnik V vaccine had reduced neutralizing capacity against the B.1.351 and E484K mutant spike, respectively.
The UK VOC is not very resistant to pre-existing or vaccine-induced antibodies, but the B.1.351 variant does show marked resistance. In fact, 8 of 12 samples were unable to reach IC90 at the highest possible serum concentration.
One neutralized the UK variant but none of the other three. These findings are of particular concern because all three VOCs carry the N501Y RBD substitution that confers increased affinity for the ACE2 receptor.
E484K mutation is present in 17 lineages detected in South America and is the only substitution in the RBD in many of them. Its role in the immune evasion of many RBD-directed monoclonal antibodies is already known. However, the current study shows that it is also associated with escape from polyclonal antibodies.
This resistance is competitive and is absent at higher serum concentrations. This is not the case with the set of mutations that defines the B.1.351 variant, which escapes neutralization with undiluted serum, as shown by the dose-response curve.
The study shows that the serum neutralization profile of any spike variant can be more fully described by its IC50 relative to the wildtype spike, and the dose-response slope.
While the Sputnik V vaccine probably protects against severe COVID-19 following infection by SARS-CoV-2 VOCs, it is problematic that B1.351, as well as all E484K-bearing mutants, is resistant to neutralization by sera elicited by this vaccine.
However, Fc-mediated effector functions of antibodies may also be instrumental in the protective efficacy of binding antibodies in vivo, even without neutralization of viral entry. Moreover, this study does not capture cell-mediated immunity to multiple epitopes.
“Taken together, our data argue that surveillance of the neutralizing activity elicited by vaccine sera will be necessary on an ongoing basis.”
Knowing which variants are still able to spread among vaccinated and naturally immune individuals will help decide if vaccines need to be upgraded in order to contain such transmission and help bring the pandemic to a quicker end.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources