There remains a limited amount of data on the comparative severity of illness among adult inpatients with coronavirus disease 2019 (COVID-19) caused by the Omicron or Delta variants of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A new study published on the preprint server medRxiv* assessed the disease severity of hospitalized adult patients with COVID-19 through the use of three different health outcomes.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Introduction
The SARS-CoV-2 Delta variant emerged in March 2021 and subsequently led to a devastating new wave of COVID-19 cases worldwide. In the United Kingdom, COVID-19 cases rose rapidly, first as a result of the Delta variant and then, from November 2021 onwards, because of the Omicron variant. In fact, the SARS-CoV-2 Omicron variant caused 95% of all U.K. cases by the end of December 2021.
In the current study, the researchers from University of Bristol and Pfizer Ltd explored disease severity considering that the hospitalization rate during the Omicron wave was much lower as compared to previous waves. Notably, the current study was conducted after COVID-19 vaccines were proven to be effective in preventing hospitalization due to Omicron infection. Thus, the reduced severity of Omicron could be due to the lower pathogenicity of the variant or extensive vaccine coverage throughout the U.K.
To ensure that their analysis was not biased due to widespread vaccination, the presence of underlying medical conditions, frailty, age, and pathogenicity, the scientists used three measures of severity. These measures included the lung function index (FiO2) greater than 28%, a World Health Organization (WHO) outcome score exceeding five, and a hospital length of stay (LOS) of more than three days following admission. These measures were assessed for both Omicron and Delta patients while compensating for age, frailty, and vaccination status.
Study findings
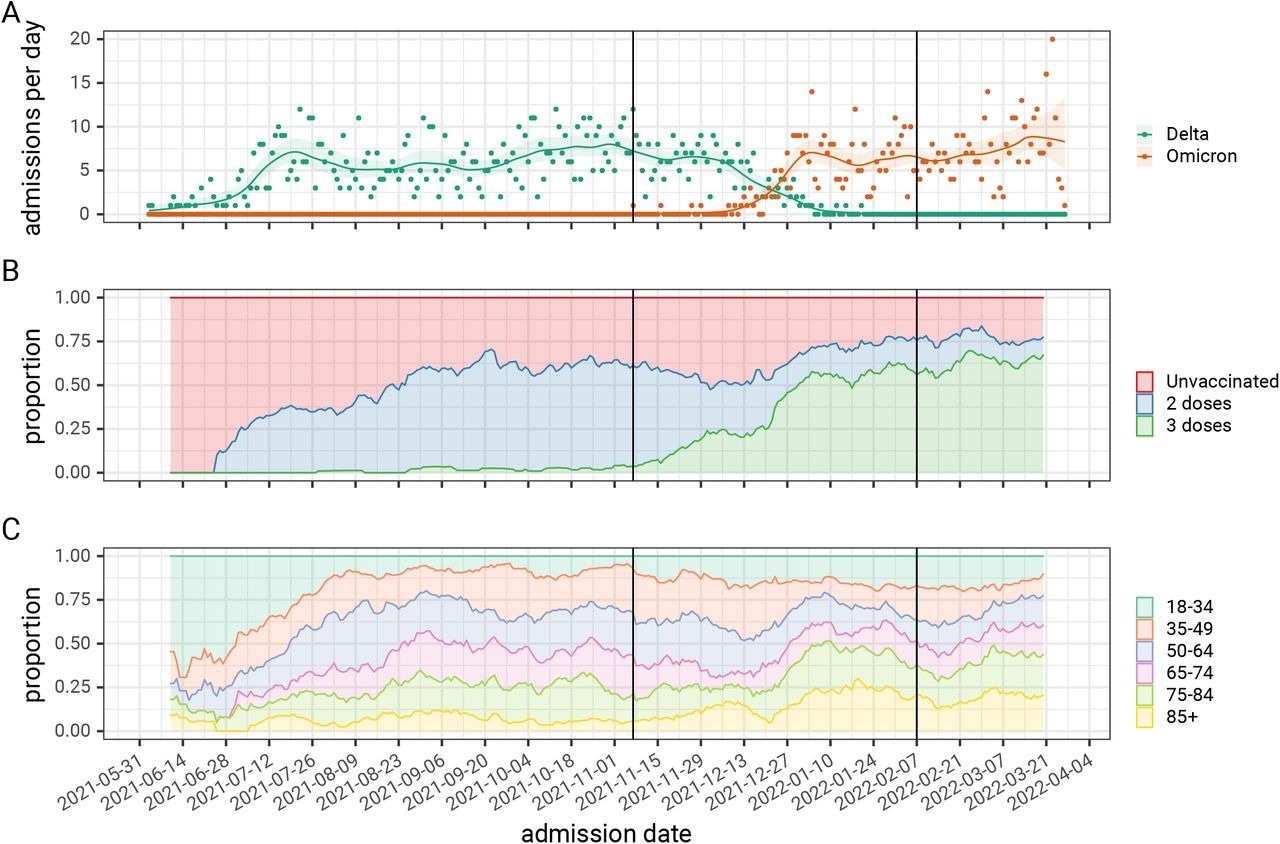
Omicron inpatients were found to be older at 71 years as compared to 58 years among Delta inpatients. Furthermore, adult inpatients diagnosed with the SARS-CoV-2 Omicron variant were more likely to have received a third booster dose, as well as have underlying medical conditions, as compared to Delta inpatients. Omicron hospitalization rates rose with time and eventually surpassed Delta rates by the end of December 2021.
There was a shift in the median age, from younger patients to those of older age, in late December 2021, which is when Omicron admissions increased. Despite being older and frailer, the outcomes of these patients were less severe than those diagnosed with the Delta variant, except in patients aged 85 years or above. Similarly, LOS decreased with Omicron, except for those aged 70 or above.
The detailed breakdown of the three selected indicators of the severity of hospital admission stratified by SARS-CoV-2 variant, and the comparison of three binary indicators of hospital burden and their relationship to SARS-CoV-2 variant and patient age, for patients admitted to hospital.
Omicron-related admissions were about 60%, 70%, and 20% less likely to require high-flow oxygen, positive pressure ventilatory support, or more critical care, respectively. The likelihood of LOS exceeding three days was 20% lower with Omicron.
This association between Omicron and less severe disease was observed in both vaccinated and unvaccinated patients. Even so, vaccinated patients showed lower rates of high-flow oxygen requirement by over 20%, as well as even greater reductions in the need for higher-grade interventions by almost 40%.
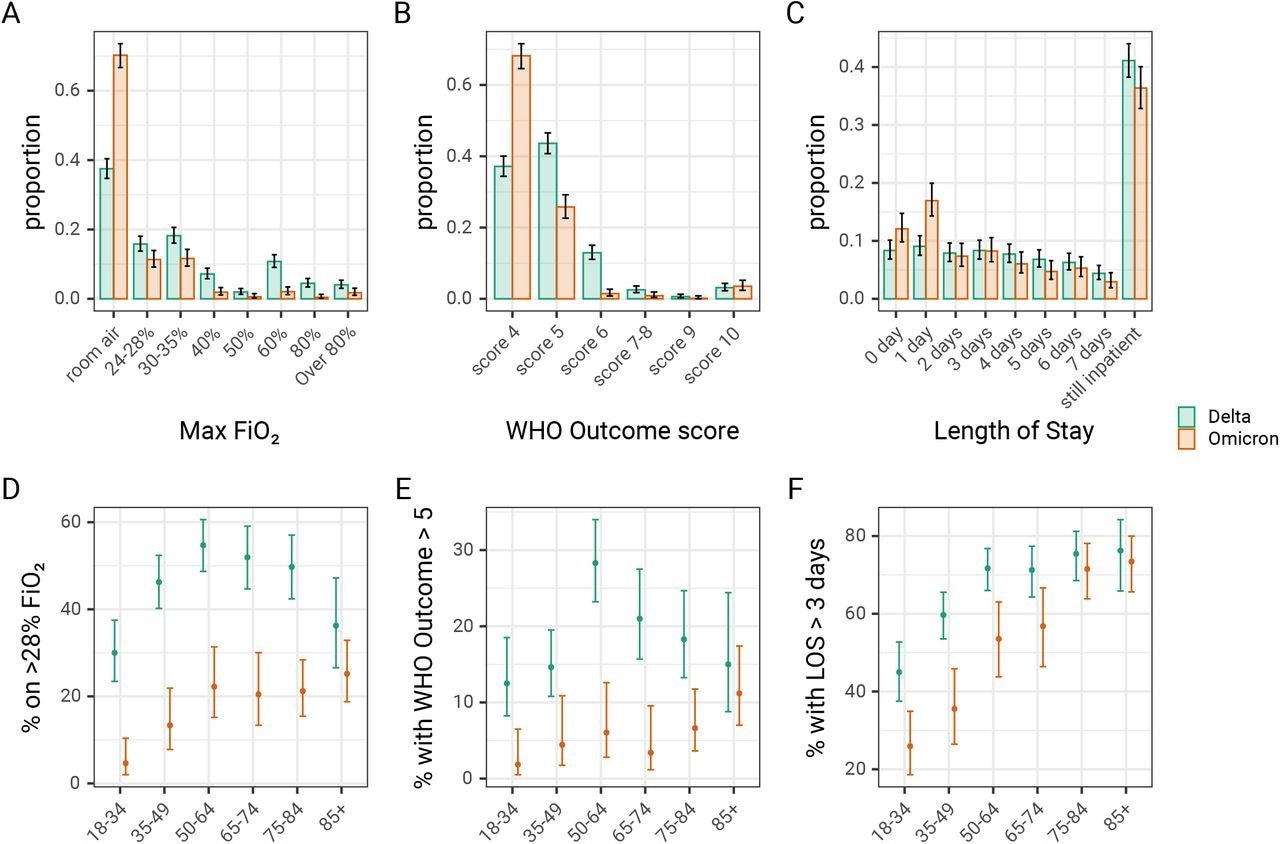
The distribution of patients (A) requiring different peak levels of oxygen supplementation, (B) with different ventilation requirements as defined by the WHO outcome or clinical progression score, and (C) with different lengths of stay. The proportion of patients who (D) require high flow oxygen >28% FiO2, (E) has a WHO outcome score>5 (requiring NIPPV), and (F) have a hospital length of stay greater than three days, as assessed on the seventh day following admission. Error bars show 95% binomial confidence intervals for each outcome, compared to other outcomes. FiO2, Fraction of inspired oxygen; LOS, length of stay; NIPPV, non-invasive positive pressure ventilation
Implications
The study findings indicate that the SARS-CoV-2 Omicron variant is associated with less severe infection as compared to the Delta variant, thus corroborating earlier reports.
The researchers anticipate that their findings could contribute to future hospital care and service planning assessments. For instance, the total capacity of mechanical and non-invasive ventilation and oxygen could be planned using these and similar reports.
Nevertheless, the Omicron variant is demonstrably more transmissible than any other SARS-CoV-2 variant to date. As a result, the SARS-CoV-2 Omicron variant leads to much higher infections, which could mean that a much lower proportion of hospitalizations could still have a significant impact on healthcare systems.
One in five Omicron patients require supplemental oxygen, 6% require positive pressure ventilation, and 4% die of the infection. Thus, very high infection rates due to this variant could inevitably overwhelm hospitals. The risk that hospital and other healthcare staff may be infected and subsequently need to quarantine also increases the likelihood of staff shortages during Omicron-related surges.
The reductions in oxygen requirements and lower WHO outcome scores suggests that exhaustion of oxygen supplies or high dependency care beds are less likely to be seen in large waves of community Omicron infection than was the case with Delta and other previous variants. Vaccination is seen to reduce these risks further.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Hyams, C., Challen, R., Marlow, R., et al. (2022). Severity Of Omicron (B.1.1.529) and Delta (B.1.1.617.2) SARS-Cov-2 Infection Among Hospitalised Adults: A Prospective Cohort Study. medRxiv. doi:10.1101/2022.06.29.22277044. https://www.medrxiv.org/content/10.1101/2022.06.29.22277044v1.full.pdf.
- Peer reviewed and published scientific report.
Hyams, Catherine, Robert Challen, Robin Marlow, Jennifer Nguyen, Elizabeth Begier, Jo Southern, Jade King, et al. 2023. “Severity of Omicron (B.1.1.529) and Delta (B.1.617.2) SARS-CoV-2 Infection among Hospitalised Adults: A Prospective Cohort Study in Bristol, United Kingdom.” The Lancet Regional Health – Europe 25 (February). https://doi.org/10.1016/j.lanepe.2022.100556. https://www.sciencedirect.com/science/article/pii/S2666776222002526.