A groundbreaking soft robotic heart could transform treatment for end-stage heart failure, bringing us closer than ever to fully functional, biocompatible artificial organs.
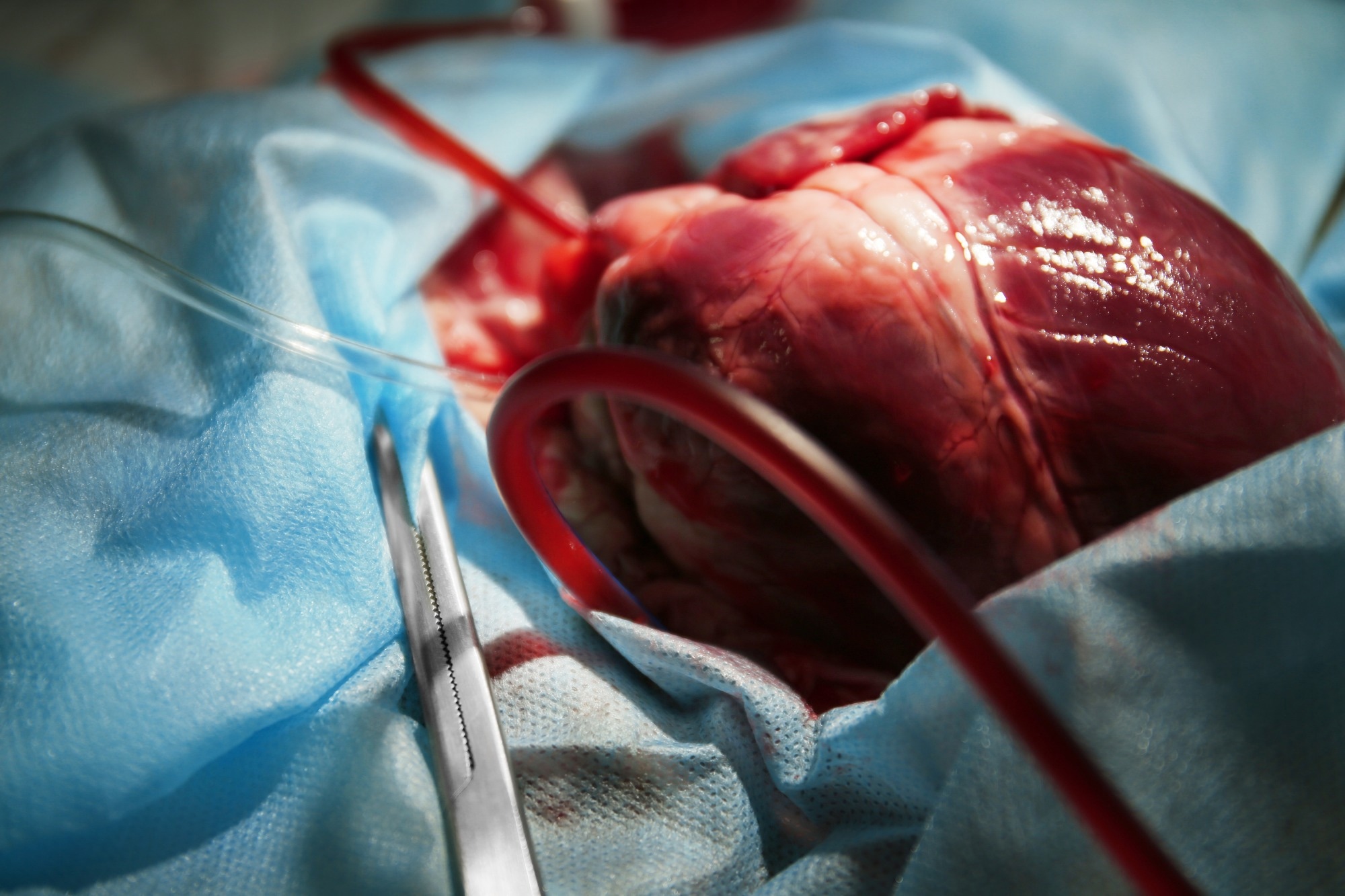 Study: A soft robotic total artificial hybrid heart. Image credit: Africa Studio/Shutterstock.com
Study: A soft robotic total artificial hybrid heart. Image credit: Africa Studio/Shutterstock.com
Researchers developed a total artificial hybrid heart powered by soft robotics, which may open new horizons in heart failure and transplantation medicine. The article providing the first proof-of-concept of this novel discovery is published in the journal Nature Communications.
Background
End-stage heart failure is associated with a high mortality rate. The condition is treatable through heart transplantation; however, the unavailability of donor hearts is the principal disadvantage. This limitation has led to the development of total artificial hearts and left ventricular assist devices.
These artificial devices exhibit poor biocompatibility as the materials used to design them are not derived from the patient’s body. Moreover, these devices work non-physically to circulate blood throughout the body. These factors can induce blood clot formation, which can subsequently lead to complications related to blood flow.
Percutaneous drivelines, which are required for powering and connecting currently available heart devices to an external source, exhibit a high infection risk and significantly impact a patient’s quality of life. These complications largely restrict the clinical use of currently available total artificial hearts.
In the current study, researchers developed a hybrid total artificial heart, wherein the pumping power comes from soft robotics to propel the blood physiologically. They named the device “Hybrid Heart”.
Hybrid Heart – Design and Working Principle
The researchers designed this new generation of total artificial hearts with the idea that the device should mimic the structure and function of the human heart. The human heart has two chambers, the left and right ventricles, which are separated by a septum (a dividing wall). The synchronous contraction of the ventricles and septum results in blood being ejected from the ventricles into circulation.
Like the human heart, the Hybrid Heart contains two artificial chambers separated by a soft pneumatic muscle (septum). The ventricles and septum are composed of nylon coated with thermoplastic polyurethane. Notably, the design also includes multiple inextensible wires arranged in a closed loop, which play a key role in mimicking the coordinated contractions of the heart by distributing forces across both ventricles.
Supramolecular coatings are applied to the thermoplastic polyurethane-coated nylon material to enhance biocompatibility.
Positive or negative air pressure is used to inflate and deflate the septum. When the septum inflates during systole, its internal diameter increases, allowing more wire to be wrapped around it. This squeezes the ventricles to eject blood, like a natural heart. When the septum deflates during diastole, the ventricles passively refill.
The specific length and number of wires around each ventricle can be adjusted to alter the cardiac output of each chamber, enabling adaptation to the requirements of different physiological conditions or diseases. This adjustability could be important for matching the device to individual patient needs, such as in cases of pulmonary hypertension.
A soft robotic actuation mechanism provides the required pressure profile to the Hybrid Heart’s septum. The actuation mechanism translates control signals into physical actions within a system. This soft robotic actuation mechanism does not depend on electronics to generate a heartbeat; instead, it autonomously and passively transforms the constant flow of a continuous air pump into pressure pulses that create the heartbeat for the Hybrid Heart.
However, the overall system also includes electronic components for power and control, especially in future fully implantable versions.
Functional Validation
The laboratory testing of the Hybrid Heart under physiological conditions revealed that the device mimics the pumping physiology of the human heart, and its left ventricle can pump 5.7 liters of blood per minute (cardiac output) at a heart rate of 60 beats per minute. Since the cardiac output of the left ventricle should be higher than the right ventricle, the cardiac output of the device’s right ventricle was set at 5 liters per minute by adjusting the length of the wires around the right ventricle.
The Hybrid Heart was further tested in animals by surgically implanting the device in the pericardial space. The device was responsible for all animal blood flow during a 50-minute testing period.
The animal test was a short-term experiment, not a long-term implant, providing an initial proof-of-concept for the device’s function in vivo.
However, in the acute animal test, the cardiac output was lower than in vitro (about 2.3 liters per minute at 65 bpm), reflecting the device's early-stage, proof-of-concept nature and expected technical limitations.
The findings revealed that the thermoplastic polyurethane-coated nylon material used in the Hybrid Heart is non-toxic, exhibits improved biocompatibility, and possesses potent anti-thrombogenic properties due to its supramolecular coatings.
Animal and in vitro tests demonstrated significant reductions in platelet adhesion and thrombosis compared to uncoated materials, supporting its potential for long-term blood compatibility.
In laboratory and animal experiments, an open pneumatic system was used for the Hybrid Heart actuation. However, a fully implantable, closed fluidic driving system has been developed for future clinical use. This system consisted of an implanted continuous-flow air pump, an air container, and a soft robotic actuation system connected to the septum in a closed circulation loop.
The closed fluidic system was integrated into a transcutaneous energy transfer system (TET) to provide electrical energy to the pump wirelessly. The external TET coil, placed on the patient’s skin, transmitted power to the subcutaneously implanted internal TET coil, while leaving the skin intact.
This approach can potentially reduce the risk of infection and enhance patients' quality of life by allowing them to temporarily detach from a power source and engage in activities such as showering or swimming freely.
The testing of this closed fluidic system revealed that upon powering the continuous flow air pump, the Hybrid Heart automatically started to beat at a heart rate of 35 bpm and produced a relatively low cardiac output compared to that produced by the traditional driving system.
This limitation was attributed to the available power from the TET system in the initial experiments, which was not a fundamental barrier to the technology. The research noted that increasing the input energy should improve cardiac output, and the researchers are currently working on this.
Additionally, the Hybrid Heart showed adaptive physiological properties. Preload and afterload sensitivity means the Hybrid Heart can adjust its output in response to changing blood pressure and volumes, like a natural heart. This is achieved passively, mimicking the Frank-Starling mechanism, whereby the heart increases production in response to increased filling without needing complex sensors or electronics.
The design also allows for the individual configuration of the device, such as altering wire length and position, tailored to meet individual patient needs.
While the proof-of-concept is promising, the work is still in its infancy. The device was built upon prototyping materials rather than medical-grade components, and further long-term animal studies will be necessary to fully validate the technology’s safety, durability, and performance.
Before any clinical application, all key components, including the fully implantable version and tissue engineering coatings, will require extensive further testing, including long-term animal studies.
Significance
The study provides the first evidence that soft robotic techniques can successfully develop a biocompatible total artificial heart capable of delivering adequate cardiac output under physiological conditions.
The Hybrid Heart developed in the study can overcome the shortcomings of currently available, total artificial hearts, potentially providing both anti-thrombogenic surfaces and support for tissue integration.
In the future, coating technology could be further developed, for example, by incorporating molecules that actively encourage the body’s cells to colonize the device and form a functional inner lining. This dual approach to reducing blood clotting and supporting the body’s tissue integration could reduce the need for lifelong anticoagulation therapy.
Although the Hybrid Heart is not yet ready for clinical use and will require further thorough testing and optimization, it demonstrates how soft robotics and biomimetic engineering can provide safer, more functional, and more adaptable artificial hearts for end-stage heart failure.
Download your PDF copy now!