Introduction
Hemorrhoids
Diverticular Disease
Anal Fissure
Ulcerative Colitis
Angiodysplasia of the Colon
Peptic Ulcers
Colon Polyps and Colorectal Cancer
Infectious Colitis
Ischemic Colitis
Medication-Induced Bleeding
Other Causes
Pediatric Considerations
Assessment and Diagnosis
Red Flags and When to Seek Help
References
Further Reading
Don’t ignore blood in your stool; knowing the causes and warning signs can help you detect hidden diseases early and protect your long-term health.
 Image Credit: luchschenF / Shutterstock
Image Credit: luchschenF / Shutterstock
Introduction
Blood in the stool may be noticed after a bowel movement or following a test arranged by a doctor. It denotes the presence of bleeding somewhere within the gastrointestinal tract, comprising the mouth, esophagus, stomach, small intestine, large intestine, and anus.
The amount of blood in the stool may be so small that it is only detected by a fecal occult blood test (FOBT) or a fecal immunochemical test (FIT), which are non-invasive screening tests that look for invisible blood in the stool. If more blood is present, it may be noticed on toilet tissue or seen as bright red blood in the stool after a bowel movement. A positive result on FOBT or FIT may indicate gastrointestinal bleeding and usually warrants further investigation, typically with colonoscopy, to determine the source. Other substances, such as iron supplements, bismuth, or certain foods (e.g., beets), can also change stool color and may sometimes mimic or mask the appearance of blood.
Bleeding from the gut may cause the stool to appear black and tarry, a condition referred to as melena. Bright red blood is referred to as hematochezia. Melena is more likely to occur when the blood originates in the esophagus, stomach or small intestine, while hematochezia is more likely when the source is the large intestine or rectum. However, very rapid upper gastrointestinal bleeding can occasionally present as hematochezia.
Rectal bleeding is relatively common, affecting up to 13–34% of individuals at some point in their lives, although less than half of those affected seek medical care. The prevalence and most likely causes of rectal bleeding vary by age, with hemorrhoids and anal fissures most common in younger adults, while diverticulosis and malignancy become more important considerations in older individuals. The risk of a serious underlying cause increases with age, family history of colorectal cancer, or the presence of other symptoms such as weight loss or anemia.
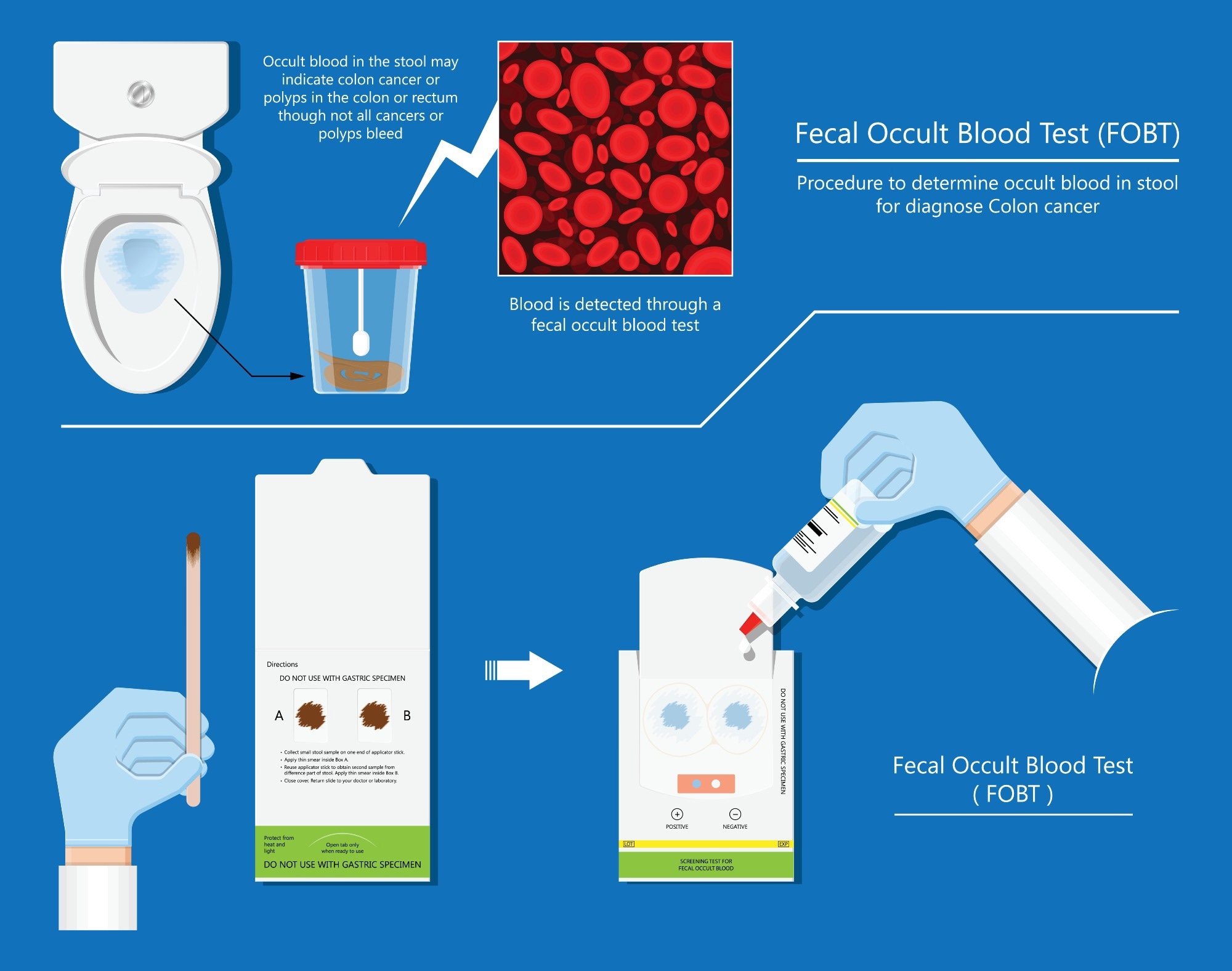 Fecal occult blood test FOBT lab stool sample, bleeding screen, risk examination, collect container, Guaiac diagnosis, sign, hemoccult smear, FIT diagnostic. Image Credit: Pepermpron / Shutterstock
Fecal occult blood test FOBT lab stool sample, bleeding screen, risk examination, collect container, Guaiac diagnosis, sign, hemoccult smear, FIT diagnostic. Image Credit: Pepermpron / Shutterstock
Some of the most common causes of gastrointestinal bleeding and blood in the stool are described below.
Hemorrhoids
Hemorrhoids are the most frequent cause of painless rectal bleeding in adults. They are swollen veins in the anus or lower rectum and often cause bright red blood on toilet tissue, dripping into the bowl, or coating the stool. Bleeding from hemorrhoids is usually painless and can occur with or without defecation. Risk factors include straining during bowel movements, chronic constipation, prolonged sitting, low fiber diet, pregnancy, and aging. Mild cases often resolve with conservative measures, such as increased fiber intake and topical treatments, while persistent cases may require procedures like rubber band ligation or surgery.
Diverticular Disease
Here, small pouches or pockets called diverticula develop in and project from the intestinal lining. They are common in older individuals and are thought to form as the result of weakening of the colonic wall over time as hard stools are passed through it.
Diverticular disease typically does not cause symptoms; however, the diverticula may become infected (diverticulitis) or bleed. Approximately 15% of individuals with this disease find that they pass blood in their stool. However, the problem does not usually cause pain and it is self-limited in around 80% of cases. Bleeding that does not clear up may require hospital monitoring, blood transfusion, or endoscopic intervention to stop bleeding.
Anal Fissure
This is a small tear or cut in the thin, moist lining of the anus, often as a result of passing a hard and/or large stool. This can cause pain and bleeding. The majority of anal fissures resolve without treatment, especially if simple changes are made such as an increased intake of dietary fiber and topical medications (like nitroglycerin ointment or calcium channel blockers), although more invasive medication or surgery is occasionally required. Anal fissures are the most common cause of blood in the stool in infants and young children.
Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease characterized by chronic inflammation and ulceration of the innermost lining of the colon and rectum. Symptoms develop gradually, but the condition can be debilitating or even life-threatening. No cure has yet been developed, but treatment with anti-inflammatory medications, immunosuppressants, or biologics is often effective in improving symptoms. Crohn’s disease, another inflammatory bowel disease, can also result in bleeding anywhere from the mouth to the anus.
Angiodysplasia of the Colon
This condition is characterized by malformed or dilated aging blood vessels in the colon, which become fragile, swell and break, resulting in bleeding. The bleeding may be slow, eventually causing anemia, or it may be severe and require hospital monitoring and blood transfusion. Treatment often involves endoscopic cauterization.
Peptic Ulcers
A peptic ulcer is a sore found in the stomach or duodenum. It is often the result of infection by the organism Helicobacter pylori, or the ongoing use of anti-inflammatory drugs such as ibuprofen and aspirin which can damage the protective mucosal lining. The most common symptom is stomach pain, which can be exacerbated by stress or consuming spicy foods. Peptic ulcers are the most common cause of upper GI bleeding, which may present as melena or, if severe, as hematochezia. Treatment focuses on acid suppression and eradicating H. pylori if present. Individuals who use both NSAIDs and anticoagulants are at particularly increased risk for ulcer-related bleeding.
Colon Polyps and Colorectal Cancer
Polyps are small growths that form on the colon lining. They are usually benign, but can increase in size, start to bleed and potentially become cancerous, leading to colon cancer. This can be fatal if the cancer is not discovered until it is advanced. Detected polyps are typically removed during colonoscopy (polypectomy).
Rectal cancer is cancer that arises in the last section of the colon. Colon and rectal cancers are together referred to as colorectal cancers. Anyone can develop colon polyps, although people aged 50 years and older are at an increased risk, along with people who smoke, are overweight, or have a family history of colon polyps or colon cancer.
Colorectal cancer and polyps often cause bleeding that cannot be seen with the naked eye. It is therefore important that regular screening for this disease be done, since polyps found early on in the course of disease can usually be removed so that cancer is prevented from developing in a number of cases. Fecal immunochemical tests (FIT) and colonoscopy are standard screening tools used to detect occult bleeding and early colorectal cancer.
Infectious Colitis
Bacterial, viral, or parasitic infections—including Salmonella, Shigella, Campylobacter, Entamoeba histolytica, Escherichia coli, Clostridium difficile, and sexually transmitted infections—can cause inflammation of the colon (colitis), leading to blood in the stool. Infectious colitis may present with diarrhea, abdominal pain, and fever in addition to rectal bleeding. Treatment targets the specific pathogen.
Ischemic Colitis
This condition occurs when blood flow to part of the colon is reduced, usually in older adults or those with risk factors for vascular disease like hypertension, diabetes, or atherosclerosis. Ischemic colitis typically causes sudden abdominal pain followed by rectal bleeding and can be associated with other chronic diseases.
Medication-Induced Bleeding
Medications such as non-steroidal anti-inflammatory drugs (NSAIDs), aspirin, anticoagulants (such as warfarin), and antiplatelet agents can directly irritate the GI tract or impair clotting, increasing the risk of gastrointestinal bleeding, especially in people with other risk factors. Iron supplements and bismuth can also change stool color, sometimes mimicking bleeding. The risk of bleeding is amplified when these medications are used together or in individuals with underlying gastrointestinal conditions.
Other Causes
Radiation proctitis (bleeding after pelvic radiation therapy), angiodysplasia (vascular malformations), and rare causes such as Meckel’s diverticulum can also be responsible. Intussusception, a condition where part of the intestine telescopes into itself, can cause blood in the stool, particularly in infants and young children.
Pediatric Considerations
In children, the causes of blood in the stool differ from adults and can include anal fissures (most common), juvenile polyps, Meckel’s diverticulum, intussusception, milk protein allergy in infants, and infections. Significant or recurrent bleeding in children warrants specialist evaluation. The likelihood of each cause varies by age group, and clinical context should guide investigation.
Assessment and Diagnosis
A thorough medical history and physical examination are essential to determine the likely source and cause of bleeding. Important points include onset, quantity, duration and frequency of bleeding, associated symptoms (such as pain, weight loss, or change in bowel habits), medication use, and family or personal history of gastrointestinal disease or cancer.
Laboratory testing (including a complete blood count and coagulation profile) and endoscopic evaluation (upper endoscopy (EGD), anoscopy, sigmoidoscopy, or colonoscopy) are often required. Imaging studies such as CT angiography or nuclear scans may be used in selected cases. The choice of initial diagnostic test often depends on the patient's age, risk factors, and whether bleeding is suspected to originate from the upper or lower GI tract.
Red Flags and When to Seek Help
Urgent medical evaluation is recommended for blood in the stool if accompanied by large volume bleeding, dizziness, fainting, low blood pressure, severe abdominal pain, fever, weight loss, anemia, or known risk factors for colorectal cancer. Any new rectal bleeding in individuals over age 50 or with a family history of colorectal cancer should prompt early evaluation, even if symptoms are mild.
References
- Angiodysplasia of the colon: MedlinePlus Medical Encyclopedia. (n.d.). Medlineplus.gov https://medlineplus.gov/ency/article/000238.htm
- National Institute of Diabetes and Digestive and Kidney Diseases. (2017, December). Your Digestive System & How It Works. NIDDK. https://www.niddk.nih.gov/health-information/digestive-diseases/digestive-system-how-it-works
- Wilson ID. Hematemesis, Melena, and Hematochezia. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 85. Available from: https://www.ncbi.nlm.nih.gov/books/NBK411/
- Does Blood in Stool Mean Cancer? (2024). Cancer.org. https://www.cancer.org/cancer/diagnosis-staging/signs-and-symptoms-of-cancer/blood-in-stool.htm
- Orpen-Palmer, J., & Stanley, A. J. (2022). Update on the management of upper gastrointestinal bleeding. BMJ Medicine, 1(1).DOI:10.1136/bmjmed-2022-000202
- NHS Choices. (2019). Bleeding from the bottom (rectal bleeding). NHS. https://www.nhs.uk/conditions/bleeding-from-the-bottom-rectal-bleeding/
- Sabry AO, Sood T. Rectal Bleeding. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563143/
- Bowel Cancer UK. (2019, July 24). Signs & symptoms | About bowel cancer. Bowel Cancer UK. https://www.bowelcanceruk.org.uk/about-bowel-cancer/symptoms/
- Haemorrhoids (piles) symptoms and treatments. (n.d.). Www.nhsinform.scot. https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/haemorrhoids-piles/
Further Reading
Last Updated: Jun 6, 2025