Insulin is a hormone that is important for metabolism and utilization of energy from the ingested nutrients - especially glucose.
Insulin chemistry and etymology
Insulin is a protein chain or peptide hormone. There are 51 amino acids in an insulin molecule. It has a molecular weight of 5808 Da.
Insulin is produced in the islets of Langerhans in the pancreas. The name insulin comes from the Latin ''insula'' for "island" from the cells that produce the hormone in the pancreas.
Insulin's structure varies slightly between species of animal. Both porcine (from pigs) and bovine (from cows) insulin are similar to human insulin but porcine insulin resembles human insulin more closely.
What does insulin do?
Insulin has several broad actions including:
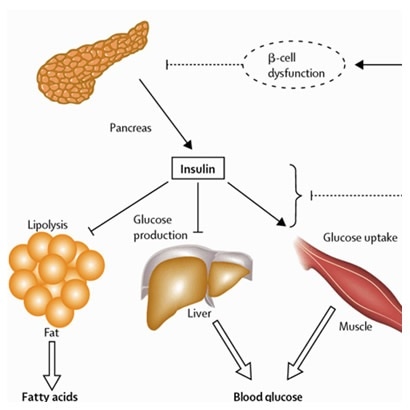
- It causes the cells in the liver, muscle, and fat tissue to take up glucose from blood and convert it to glycogen that can be stored in the liver and muscles
- Insulin also prevents the utilization of fat as an energy source. In absence of insulin or in conditions where insulin is low glucose is not taken up by body cells, and the body begins to use fat as an energy source
- Insulin also controls other body systems and regulates the amino acid uptake by body cells
- It has several other anabolic effects throughout the body as well
Secretion of insulin
Insulin is synthesized in significant quantities only in beta cells in the pancreas. It is secreted primarily in response to elevated blood concentrations of glucose. Insulin thus can regulate blood glucose and the body senses and responds to rise in blood glucose by secreting insulin.
Other stimuli like sight and taste of food, nerve stimulation and increased blood concentrations of other fuel molecules, including amino acids and fatty acids, also promote insulin secretion.
What happens when there is insufficient insulin?
Since insulin controls the central metabolic processes, failure of insulin production leads to a condition called diabetes mellitus. There are two major types of diabetes – type 1 and type 2.
Type 1 diabetes occurs when there is no or very low production of insulin from the pancreatic beta cells. Patients with Type 1 diabetes mellitus depend on external insulin (most commonly injected subcutaneously) for their survival.
In type 2 diabetes mellitus the demands of insulin are not met by the amount produced by the pancreatic beta cells. This is termed insulin resistance or ''relative'' insulin deficiency. These patients may be treated with drugs to reduce their blood sugar or may eventually require externally supplied insulin if other medications fail to control blood glucose levels adequately.
Further Reading
Last Updated: Jun 20, 2023