Nearly three million people in the United States experience traumatic brain injury (TBI) every year, and there are no pre or post-TBI treatment options available. Now, a new novel therapy shows promise in preventing brain damage after traumatic brain injury.
A team of researchers at the University of Texas Health Science Center at San Antonio may have invented a promising experimental treatment provided for mice after traumatic brain injury (TBI). After the treatment, there was reduced damage nearly to the levels of mice that never had a TBI.
Published in the Journal of Cerebral Blood Flow and Metabolism, the study shows that brain damage can be prevented after TBI, which can open the doors for effective and simple treatments to be implemented in emergency rooms or by first aid responders shortly after a brain injury.
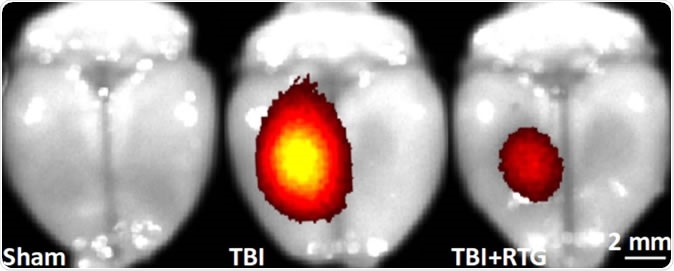
Red and yellow areas show sites of cell death in the mouse brain. The brain at left has no traumatic brain injury (TBI). The brain at center is post-TBI. The brain at right is post-TBI and treated with the novel therapy; cell death is nearly abolished. Image Credit: Mark S. Shapiro, Ph.D., UT Health San Antonio
No current treatment for TBI
Today, there is no known treatment for traumatic brain injury, which is caused by a blow, jolt, bump, or penetration to the head disrupting normal brain function. After a TBI, the brain may have dangerous inflammation, causing nerve cell death. Moreover, the blood-brain barrier, which is important in maintaining normal brain function, starts to break down.
Usually, patients with TBI manifest any period of loss of consciousness, loss of memory especially of events before or after the injury, and neurological deficits such as loss of coordination and balance, change in speech, muscle weakness, and altered mental state.
In worse cases, patients may have seizures and they may die if the condition is left untreated or if immediate care isn’t provided. In the long term, patients who had TBI may suffer from complications such as paralysis, Alzheimer’s disease, and other types of dementia.
TBI contributes to a considerable number of deaths, including many cases of permanent disability. About 2.5 million TBI cases occurred in 2010 alone, and each day, 138 people in the United States die from injuries, including TBI. Approximately 53,000 people had died of TBI-related injuries in the same year, the Centers for Disease Control and Prevention (CDC) reports.
At present, there are no current treatments for TBI to prevent brain damage. Medications and surgery are usually done to minimize additional damage to brain tissues. Emergency surgery is performed to remove clotted blood, repair skull fractures, and relieve pressure in the skull. However, a TBI treatment to prevent brain damage right after the injury hasn’t been developed yet, not until now.
The novel therapy for TBI
After the mice suffered TBI, about 40 percent experienced a seizure within one week of the injury. Many of the mice models continued to experience seizures for years, leading to epilepsy disease. What happened to the mice is like what happens in humans. After TBI, humans may also experience changes in emotional state and cognitive dysfunction.
“KCNQ2-5 voltage-gated K+ channels underlie the neuronal “M current”, which plays a dominant role in the regulation of neuronal excitability. Our strategy towards prevention of TBI-induced brain damage is predicated on the suggested hyperexcitability of neurons induced by TBIs, and the decrease in neuronal excitation upon pharmacological augmentation of M/KCNQ K+ currents,” the researchers explained in the study.
To prevent abnormal electrical activity in the brain, the new therapy boosts the activity of “M-type” KCNQ potassium ions channels, which are proteins that can stop sudden and uncontrolled electrical currents in nerve cells.
After a TBI, abnormal electrical currents start even before the occurrence of seizures. The new therapy aims to stop and counteract the occurrence of abnormal currents in the brain, hence, stopping the chain of events that might lead to brain damage.
After the treatment of mice models who had TBI, there were no observed seizure bouts.
"We need treatments that alter some of the disabling consequences of TBI. Current antiseizure medications don't prevent the development of post-traumatic epilepsy,” Dr. Jose E. Cavazos, an epilepsy specialist at UT Health San Antonio, said. “Our study examined this critically important therapeutic gap and proposes a novel pharmacological intervention shortly after TBI that might prevent post-traumatic epilepsy,” he added.
The new therapy, if developed for humans, it’s a breakthrough treatment not only for TBI patients but also for those who have seizure disorders. In fact, about 6 percent of all epilepsy cases are triggered by trauma to the head.
"Think about the possibility of taking medication shortly after the injury and preventing disabling epileptic seizures months to years later," Dr. Cavazos added.
At present, experts are evaluating the new therapeutic approach for its development for humans. They will test the therapy’s suitability in humans, which include examinations for its stability, safety, chemical properties, and effects on the other organs of the body, including the heart.
Journal reference:
Vigil, F. A., Bozdemir, E., Bugay, V., Chun, S. H., Hobbs, M., Sanchez, I., … Shapiro, M. S. (2019). Prevention of brain damage after traumatic brain injury by pharmacological enhancement of KCNQ (Kv7, “M-type”) K+ currents in neurons. Journal of Cerebral Blood Flow & Metabolism. https://doi.org/10.1177/0271678X19857818, https://journals.sagepub.com/doi/10.1177/0271678X19857818