A new study published in the open-access journal PLOS Pathogens in March 2020 reports the possible use of the bacteria Gardnerella found in the cervix and vagina of women with Human papillomavirus (HPV) infection, as a marker of precancerous change. The findings could help to find new methods of treatment that involve inducing changes in the microbiome to arrest the course of the disease.
.jpg)
Microscopic diagnosis of bacterial vaginosis. Vaginal secretions contain epithelial cells, so-called clue cells covered with bacteria Gardnerella vaginalis, 3D illustration. Image Credit: Kateryna Kon
Human papillomavirus infection
HPV infection is among the most common sexually transmitted infections and causes cervical cancer in a small proportion of cases. However, it is not known why only a small percentage of cases progress to cancer. The current study was motivated by the need to understand how the cervicovaginal microbiome affects the progression of HPV infection to a precancerous state.
The cervicovaginal microbiome
Some of the factors associated with variation in the outcome of high-risk HPV infections include smoking, the use of oral contraceptives, and parity. However, the immune response is also essential, as well as the immune genes related to the immune response, such as the human leukocyte antigen (HLA) system.
Additionally, the chemical and microbial environment of the cervix and vagina may also affect the progression of HPV infection. In general, the cervix and vagina are characterized by an abundance of Lactobacilli of certain species (Lactobacillus crispatus, Lactobacillus iners, Lactobacillus gasseri or Lactobacillus jensenii), or of multiple microbes. The former is associated with good health outcomes, lower risk for sexually transmitted infections, and preterm births.
Many studies have shown that a more diverse microbial flora is associated with increased abnormalities of the cervix as well as a higher prevalence of high-risk HPV infections.
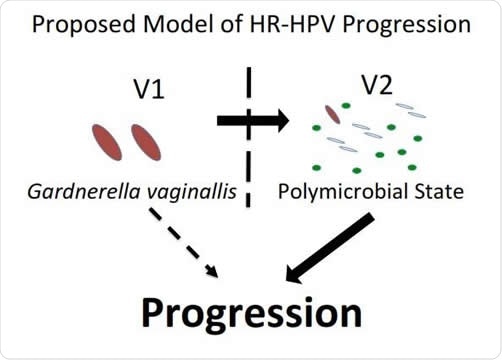
Model of HPV and microbiome interactions. Image Credit: PLOS Pathogens
The study
The current study has a longitudinal design, with cervicovaginal microbiome samples from a prospective cohort being followed up to detect any link between the microbiome and the progression of the HPV lesion to precancerous conditions of the cervix.
The researchers looked at 273 women aged 18-25 years with a high-risk HPV infection who were taking part in the Costa Rica HPV Vaccine Trial. The cervical samples were tested to obtain a picture of the microbiome and how it affects the progression to precancer, viral persistence, and viral clearance.
The findings
the researchers found four different types of bacterial communities, one each dominated by the bacterial species Lactobacillus iners in 27%, L. crispatus in 15% of samples, and Gardnerella vaginalis in 17%. In approximately 41% of cases, the microbiome was extremely diverse.
The study showed that high-risk HPV infections were cleared faster and more completely when there was an abundance of Lactobacillus iners. On the other hand, high-risk HPV progression is marked by the dominance of Gardnerella vaginalis bacteria. Apparently, Gardnerella causes a persistent HPV infection to proceed to precancer by inducing increased diversity of the cervicovaginal bacterial spectrum. This could be by inducing local immunosuppression, or alternatively a microenvironment with a distinct bacterial profile. This is supported by older studies showing differences in the immune microenvironment between the precancerous lesions that progress and those that clear entirely.
Other species associated with progression are those that are isolated from samples taken from women with bacterial vaginosis, such as Prevotella amnii and Anaerococcus prevotii. About 3.8% of fungal species were also associated with progression to precancer.
Implications
These findings suggest that the presence of Gardnerella, as well as the resulting diversity of cervicovaginal bacterial species, can be used as biomarkers to pick up those among the women infected with high-risk HPV strains who may progress to precancerous states. According to the study, “The investigators prospectively demonstrate that progression of a persistent high-risk HPV infection to cervical precancer is in part explained by unique features of the cervicovaginal microbiota.”
The paper goes on to explain, “We have identified distinct microbial biomarkers that either protect or promote the progression of an HR-HPV infection to CIN2+ lesions. These factors [might]act to suppress (in the case of progression) or activate (in the case of clearance) a localized immune response, which in turn influences the natural history of HR-HPV infection.”
Moreover, if future studies show that the microbiome of the cervix and vagina plays a causative role in the progression of persistent HPV infection to precancer, it may lead to the therapeutic induction of alterations in the cervicovaginal microbiome such as to produce local immunity and keep the disease from progressing.
Journal reference:
Usyk M, Zolnik CP, Castle PE, Porras C, Herrero R, Gradissimo A, et al. (2020). Cervicovaginal microbiome and natural history of HPV in a longitudinal study. PLoS Pathog 16(3):e1008376. https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1008376