The wide range of manifestations of COVID-19 has continued to baffle investigators. Now, a new study published on the preprint server medRxiv* in June 2020 shows that blood proteins in COVID-19 patients change over time, and these can possibly predict or reflect the severity of disease. More, they may present targets for treatment.
At present, reliable disease markers are not available either to predict the progression of the infection to severe or critical disease. However, these patients often demonstrate a cytokine storm and a deficiency of lymphocytes. Excessive inflammatory cytokine levels are related to the rapid worsening of the illness or a poor therapeutic response. Thus, it becomes essential to distinguish predictive markers to begin treatment during the stage when the disease is potentially reversible.
The Study: Protein-Severity Correlation
The current study aims at developing a protein profile that can distinguish mild, moderate, and severe COVID-19, and also detect other markers of central nervous system injury in the blood to confirm the occurrence of such a viral impact on the CNS.
As expected, mild infection occurred at significantly younger ages, and females were significantly under-represented in the critical or severe infection groups. Also, the number of days since symptom onset was much higher with mild vs. severe or critical infection.
The researchers from King's College London, University of Gothenburg and Sahlgrenska University Hospital measured 368 proteins in each of 87 samples, comprising 92 proteins each from cardiovascular, immune, inflammatory, and neurological compartments. The final analysis consisted of 355 proteins, of which 344 were unique.
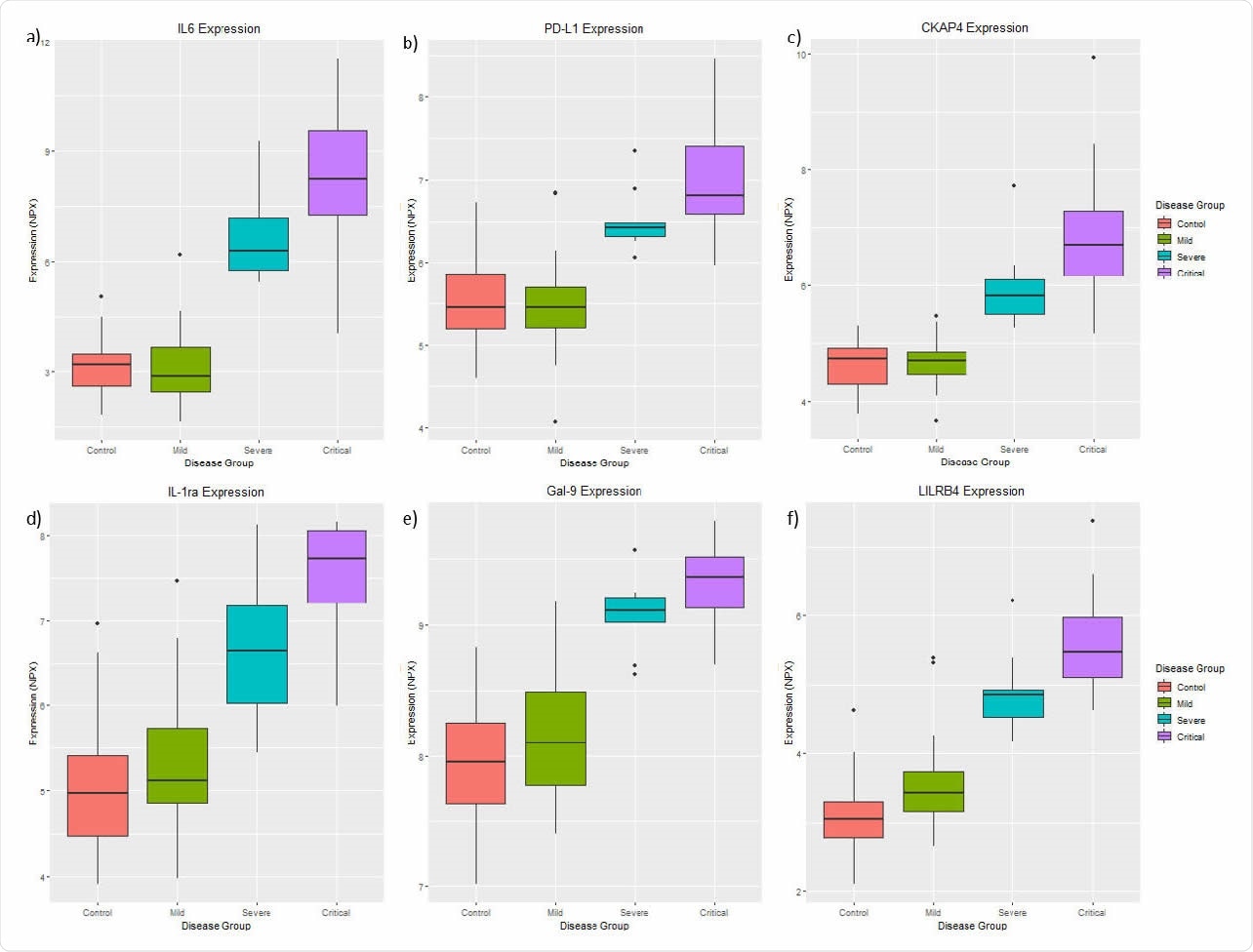
Six proteins a) IL6, b) PD-L1, c) CKAP4, d) IL-1ra e) Gal-9 and f) LILRB4 are consistently differentially expressed between the control, the mild, the severe and the critical symptom groups after controlling for age, gender, and “days since symptom onset”, suggesting these proteins may be associated with disease severity.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Protein Pattern Changes with Infection
When the cases (mild, moderate, or severe COVID-19) were analyzed vs. the controls, the researchers found that 269 proteins showed significantly different expression in cases. Among these, 120 were expressed at higher levels, and the rest at lower levels, in infected patients.
Thus, more than three-fourth of proteins in this study show significant changes in cases compared to age-matched controls. The greatest difference was seen with the NF2 (neurofibromin 2) protein that was downregulated in all cases. This protein, also called the Merlin protein, acts as a tumor suppressor by inhibiting cell proliferation and regulating cell survival, apoptosis, adhesion, and motility, as well as mitogenic pathways at tight epithelial junctions. Its deficiency, therefore, causes unregulated mitogenic signaling and tumor formation.
These proteins could be mapped to 285 metabolic pathways, with the most enriched pathway being the cytokine-cytokine receptor interaction.
Six-Protein Cohort Reflects Severe COVID-19
Six proteins increased in proportion with symptom severity. None of these are found in the CNS panel. These six include IL-6, which is repeated on three of the four panels, and the consistent pattern observed in all the panels shows that it plays a critical role in COVID-19 severity.
IL-6 is an interleukin found in the inflammatory pathway, an acute phase cytokine that may mirror the inflammation caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in lung tissue. Its levels are elevated in acute respiratory distress syndrome (ARDS) in COVID-19 and may be a predictor of higher odds of mortality. Thus, this may be a marker of severe COVID-19.
The monoclonal antibody tocilizumab is an IL-6 inhibitor being used to treat rheumatoid arthritis and is being used in various settings to mitigate severe COVID-19 symptoms.
All the six proteins, namely, IL6, CKAP4, Gal-9, IL-1ra, 185 LILRB4, and PD-L1, are linked to the immune pathway. Cytoskeleton Associated Protein 4 (CKAP4) is an innate immune component, helping to anchor cellular endoplasmic reticulum.
Galectin 9 (Gal-9) is one of the beta-galactoside binding proteins that help regulate interactions between cells and between cells and the matrix. It is found to be increased in many infections.
Interleukin-1 receptor antagonist protein (IL-1ra) is an anti-inflammatory protein that is elevated in severe COVID-19. Anakinra is a recombinant form of this molecule currently used in inflammatory conditions and is being tested in COVID-19 patients.
Programmed cell death 1 ligand 1 (PD-L1) is a protein that binds to T cell receptors to inhibit T cell activation and reduce cytokine secretion. This is important to regulate the immune response and prevent autoimmunity.
Neuronal Injury in COVID-19
Simultaneously, three neuronal proteins were found to be correlated to the injury of the neurons and gliosis. Among these, Nfl protein was a marker of CNS damage in severe disease. However, the investigators suggest that the most probable reason for neurological injury in severe COVID-19 is severe respiratory failure, with CNS hypoxia, thrombosis in the smaller brain vessels, and the cytokine storm.
Implications
Despite the apparent limitations of the study, such as the lack of correlation with clinical data like comorbidities, the small sample size, and the absence of data on concomitant use of medication, it is valuable in identifying six proteins that can be markers of COVID-19 severity, and which show that viral infection triggers a cytokine storm that causes or worsens lung injury.
The study concludes, "These proteins warrant further investigation but could provide potential as early biomarkers for disease severity and may serve as potential therapeutic targets, or as biomarkers to monitor the effect of treatments to modulate the immune system or suppress the infection."

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references:
- Preliminary scientific report.
Patel, H. et al. (2020). Proteomic Blood Profiling In Mild, Severe And Critical COVID-19 Patients. medRxiv preprint. doi: https://doi.org/10.1101/2020.06.22.20137216. https://www.medrxiv.org/content/10.1101/2020.06.22.20137216v1
- Peer reviewed and published scientific report.
Patel, Hamel, Nicholas J. Ashton, Richard J. B. Dobson, Lars-Magnus Andersson, Aylin Yilmaz, Kaj Blennow, Magnus Gisslen, and Henrik Zetterberg. 2021. “Proteomic Blood Profiling in Mild, Severe and Critical COVID-19 Patients.” Scientific Reports 11 (1). https://doi.org/10.1038/s41598-021-85877-0. https://www.nature.com/articles/s41598-021-85877-0.