The COVID-19 pandemic has notably taken a more significant toll on men compared to women, in terms of both disease severity and death. Now, a new study by researchers at the Icahn School of Medicine at Mount Sinai and published on the preprint server medRxiv* in August 2020 confirms the increased risk that males have for death following COVID-19 disease while also highlighting worse outcomes in women with coronary artery disease, obesity, and hypoxia compared to men. These emphasize the need for extra care in these groups and also helps explain the sex differences seen in COVID-19.
This scanning electron microscope image shows SARS-CoV-2 (round gold objects) emerging from the surface of cells cultured in the lab. SARS-CoV-2, also known as 2019-nCoV, is the virus that causes COVID-19. The virus shown was isolated from a patient in the U.S. Image captured and colorized at NIAID's Rocky Mountain Laboratories (RML) in Hamilton, Montana. Credit: NIAID
Earlier studies showed that case fatality rates for men with COVID-19 in China were almost double those for women. Again, Italian researchers reported that over 80% of patients in intensive care were men. The reasons for this male preponderance of severe disease have been speculated to be pre-existing diseases more commonly found in men, such as cardiovascular disease or diabetes, as well as the higher expression of ACE2 and TMPRSS2 in men which are necessary for viral entry into the host cells.
However, the current researchers reasoned that the difference in risk could be due to sex-specific clinical and molecular risk factors, which have not been explored so far. This study is therefore aimed at finding risk factors that act differently in the sexes.
Finding Sex-Dependent Risk Factors
The study included over 3,000 patients in a hospital system, who had a positive COVID-19 diagnosis. Over 99% of the patients died or were discharged over the follow-up period from April 13, 2020, through June 2, 2020. The patients were male in about 60%, and somewhat equally divided between Hispanic, Non-Hispanic black, and Non-Hispanic white, with less than 5% being Asian.
Male patients had a median age of about 64 years while it was 74 years for females, and the percentage of ever-smokers was ~17% vs. 8% for men relative to women. Hypertension, diabetes, asthma or chronic obstructive pulmonary disease (COPD) and obesity were more common in women, however, at 40% (vs 33%), 26% (vs 23%), 11% (vs 7%) and 10% (vs 7%), compared to men.
Flow diagram of included patients
Other Diseases and Mortality Risk
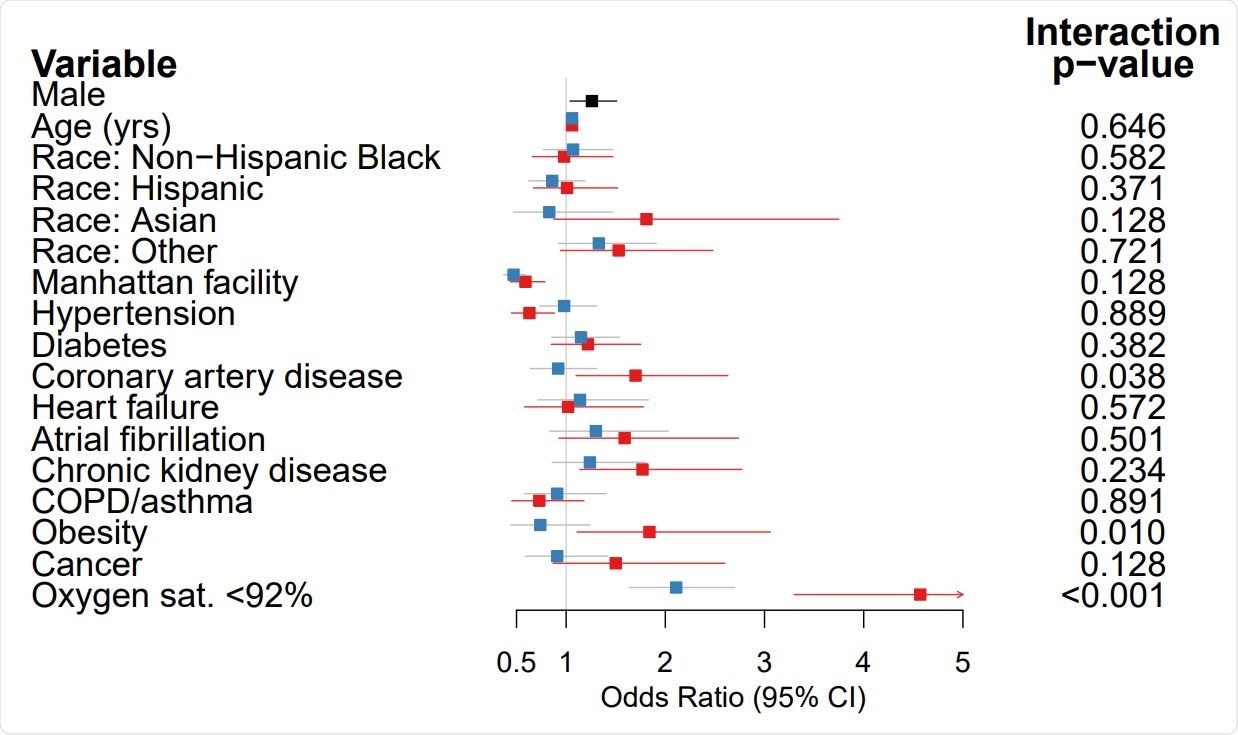
Men had 20% higher odds of death compared to women after adjusting for multiple factors like age, race, other illnesses, and the oxygen saturation at admission. The researchers found that the presence of hypoxia at admission was an independent predictor of death, conferring almost threefold higher odds of death, but not obesity or heart disease.
Next, the researchers looked at the risk of death in each of these conditions for men and women with COVID-19 separately. This showed that women with these conditions were at a higher mortality risk than men. In fact, obese men or men with heart disease had no effect on COVID-19 mortality in men but exerted a negative effect on women, with 70% to 85% higher odds of death in women with heart disease or obesity who developed COVID-19.
Concerning hypoxia at baseline, the effect was to increase the odds of death twofold in men, but over four times in women. This means that the odds of death are higher among men than in women without hypoxia, but in hypoxic individuals, the risk is the same among men and women.
Laboratory Differences and Mortality Risk
The baseline values for inflammatory markers were lower in women than in men, including white cells, procalcitonin, LDH, CRP, and ferritin. Interestingly, while ferritin levels were lower in women than in men, at ~ 500 vs. 960 ng/mL, the former had over threefold the upper limit of normal for their sex, vs. 2.4 times in men.
The proinflammatory cytokines IL-6 and IL-8 were higher in both men and women, but lower in women than in men. TNF and IL-1β were at the upper limit of normal in both.
Among all these markers, higher mortality was predicted by increased white cell count, CRP, LDH, D-dimer, and procalcitonin, as well as IL-6 and IL-8. Lower albumin levels also predicted a higher risk of death. Ferritin was linked to higher odds of mortality by ~70% in women but not in men. Procalcitonin elevation increased the odds of death in men by over twofold but not in women. LDH predicted higher odds of death in both men and women, but weakly in the former, while the odds were 2.5 times higher in women.
Among patients who had normal blood oxygenation at admission, LDH, ferritin, and IL-6 were linked to 40% to 200% higher odds of death, but not among hypoxic patients.
Implications
The study shows that women with obesity and ischemic heart disease are disproportionately at risk of death from COVID-19 compared to men, even though both sexes are at higher risk from these comorbidities.
Secondly, when it came to patients without hypoxia at baseline, both men and women were at equal risk for death. This is despite the fact that men are at higher risk for death overall. Thus, hypoxia abolishes the protective effect of the female sex. men were somewhat more likely to have hypoxia at baseline.
The researchers point out the practical application of this finding: “The risk-benefit ratio of an early-intervention agent administered to non-hypoxic patients may differ for men and women, whereas the risk-benefit ratio would not differ by sex for a therapy administered to hypoxic patients.”
Inflammation is confirmed to be a predictor of mortality. In patients without hypoxia, higher levels of LDH, CRP, IL-6, and ferritin predicted higher mortality. Thus, the study is the first to reveal the sex-dependent nature of these comorbidities and inflammatory markers. It identifies two patient subgroups who merit more careful evaluation and care.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Jun, T. et al. (2020). Sex-Specificity of Mortality Risk Factors Among Hospitalized COVID-19 Patients In New York City: Prospective Cohort Study. medRxiv preprint.
- Peer reviewed and published scientific report.
Jun, Tomi, Sharon Nirenberg, Tziopora Weinberger, Navya Sharma, Elisabet Pujadas, Carlos Cordon-Cardo, Patricia Kovatch, and Kuan-lin Huang. 2021. “Analysis of Sex-Specific Risk Factors and Clinical Outcomes in COVID-19.” Communications Medicine 1 (1). https://doi.org/10.1038/s43856-021-00006-2. https://www.nature.com/articles/s43856-021-00006-2.