As second waves of COVID-19 emerge worldwide, the need for effective vaccines is all the more imperative. Given the large pool of susceptible individuals that remain, complete relaxation of virus control measures is likely to generate further substantial waves. With several vaccines already in stage 3 clinical trials, a study by University of Warwick researchers and published on the preprint server medRxiv* in September 2020 discusses the use of computer modeling techniques in order to achieve optimal vaccine coverage.
COVID-19 mortality has been high in the elderly due to the development of severe pneumonia, sepsis, and renal failure in this cohort. It is, therefore, vital to model optimal strategies for planning and allocating resources to implement public health strategies aimed at containing the virus.
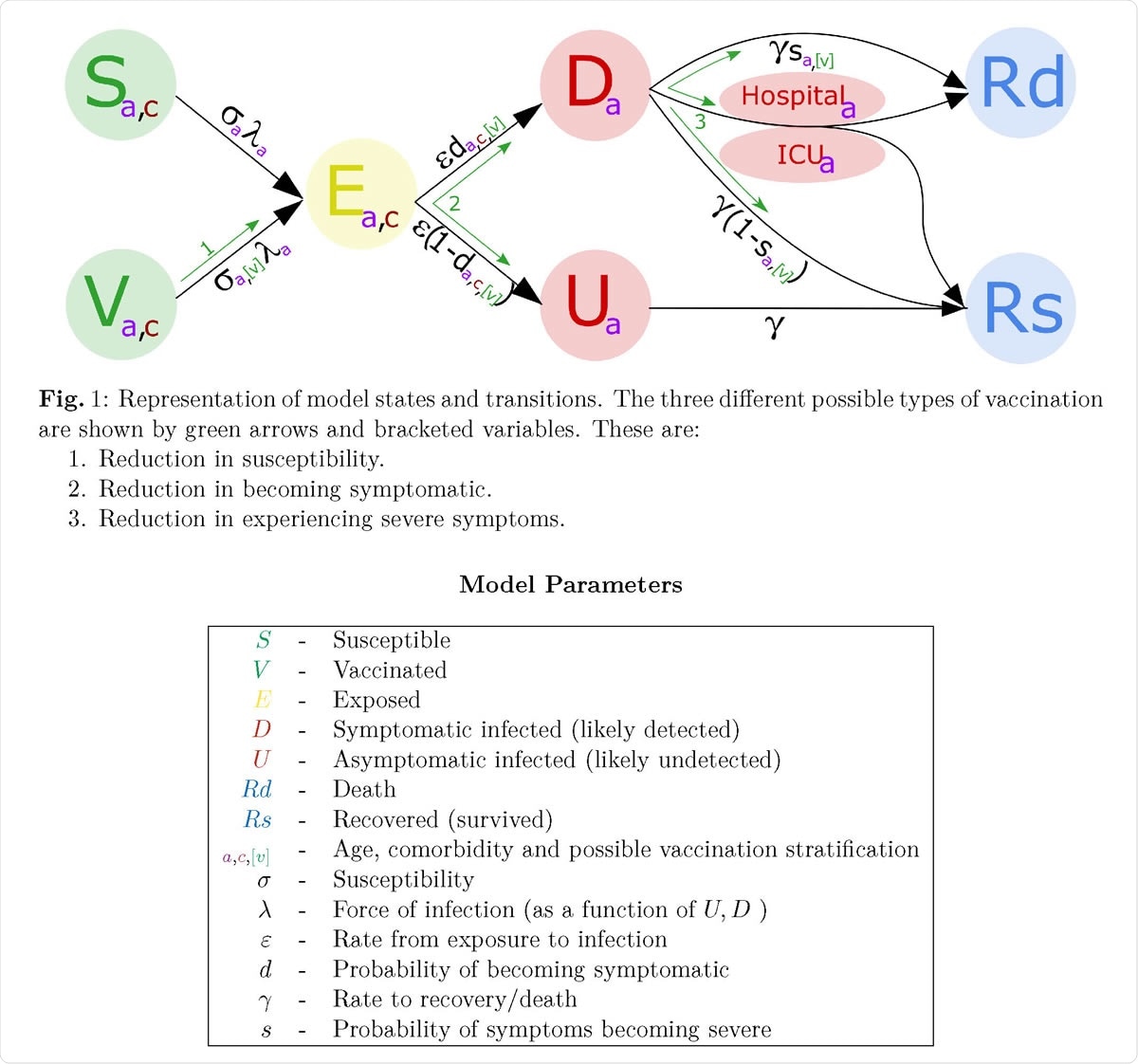
Representation of model states and transitions

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The Need to Prioritize Vaccine Administration
It is, however, uncertain how any given vaccine will actually do in the human population, even though promising results have been obtained from preclinical experiments in non-human primates and relatively small numbers of humans. For this reason, the current study focuses on adapting an earlier model of viral transmission to reflect the changes that may occur once a vaccine is in use.
Along with vaccine efficacy, how the vaccine should be used is of equal value, but has been less discussed. One question in this regard is whether those factors that drive transmission should be vaccinated first, or those at the most significant risk of severe morbidity and death.
Three Types of Vaccine
The researchers chose three types of vaccines to achieve a more comprehensive picture of the outcome that is likely to occur with the deployment of any given vaccine. Type I vaccines reduce individual susceptibility to infection; type 2 and 3 vaccines reduce symptom incidence and severity, respectively.
The first protects the individual vaccinee and limits transmission as well. The second somewhat reduces spread by reducing symptom incidence, since asymptomatic individuals may have a lower transmission risk. The third protects only the vaccinated individual from adverse outcomes.
Modeling Parameters
The current model explores the range of possible impacts in each scenario, adjusted for age-dependent variation in efficacy, as well as the scale of coverage. They also examine the criteria for the prioritization of vaccine administration.
Additionally, the researchers also assess the vaccination protocol for minimum loss of Quality-Adjusted Life Year (QALY) saved, as well as deaths averted per dose of vaccine. This approach allows a cost-benefit based evaluation of vaccine policies.
In the current study, they constructed a plot of vaccinated individuals (up to 70% in each group considered) vs. the number of deaths or QALY lost. The group that is associated with the highest reduction in either of these sequelae per dose was identified. The results were then optimized for one of these sequelae since both are closely linked.
Consistent Priority Ordering Favors Older First
When classified by various parameters, including age, the most significant effect on future mortality was found to be when the oldest were vaccinated first. Even though they are not the group most closely associated with viral spread or mobility, they are the most highly impacted by the infection in terms of severe and fatal disease.
Secondly, whatever the criteria, a targeted approach to vaccination was found to be superior to indiscriminate vaccination. On the other hand, the comorbidities which should be prioritized are dependent on age. Thus, the type of chronic disease requiring priority vaccination varied between individuals who were below 60 but beyond young adulthood and those who were over 80.
They found that the success of a vaccination program depends on five criteria:
- the type of vaccine, with type 1 being by far the most desirable;
- vaccine efficacy;
- the reproduction number;
- the vaccinated proportion concerning vaccine efficacy;
- the vaccination priority.
The authors say, “We have consistently shown that prioritizing the vaccination of the elderly is by far the most effective strategy for reducing the number of deaths in any second wave.” While this may be surprising in view of the fact that QALYs are more relevant at a younger age, it is explained by the much higher severity of disease in the elderly.
Vaccination in Healthcare Workers
The researchers also looked at the priority position of healthcare workers (HCW) on a vaccination schedule. They are not only vulnerable due to increased exposure but may drive transmission. Furthermore, they make up only 2% of the population.
For type I vaccines, HCWs are next in importance only to the most elderly age group (80 years or above) or even higher, depending on the transmission number.
Comparing Vaccine Types for Optimal Priority
The researchers then looked at the three vaccine actions and their levels of efficacy against the theoretical background of age- and disease-targeted approach to vaccination, given a low level of NPI. They also modeled what might happen if the most effective type of vaccines, namely, type 1 vaccine, was administered without any NPIs in place.
Type 1 Vaccine
The researchers found that even suboptimal type I vaccines (50% efficacy)can prevent further deaths if limited social distancing is in place (reducing the transmission number R to 1.8 or so), and 70% of the population over 20 years are vaccinated. Those aged 80 should be vaccinated first, then those with comorbidities, with the rest in order of age from the oldest downward. With more efficacy, only those above 40 years need be vaccinated.
Type 2 Vaccine
If social distancing measures maintain R at ~1.8, an effective type 2 vaccine for high-risk groups could prevent a significant number of deaths even if a second wave occurs. Vaccination of low-risk cases yields little additional benefit. The same order of priority applies here. With lower efficacy (50% or less), the scale and mortality of the second wave will mimic the first, say the researchers.
Type 3 Vaccine
Type 3 vaccines do not limit transmission, and therefore both vaccination and strict containment measures will be required to prevent sizeable future waves. The benefit of this vaccine is still likely to be significant for high-risk individuals, especially those above the age of 60 years, even considering those with chronic illnesses.
Type 1 Vaccine, No NPIs
The researchers conclude that the best vaccine would be able to arrest the pandemic by itself, allowing all NPIs to be relaxed, with a transmission number of about 2.3. This description would fit a type 1 vaccine with over 80% efficacy and covering 70% or more of the whole population. At other levels of efficacy, the percentage of vaccine coverage needed will naturally rise. Again, if more high-risk older people are immunized, fewer young people will need to be immunized.
A type 1 vaccine can be given without additional NPIs in an age-ordered fashion, without considering the presence of comorbidities, as this makes little difference to the outcome measures.
Slow vs. Fast Deployment
The above results assume rapid vaccination coverage, such that almost all eligible groups are vaccinated simultaneously. With the slower deployment, if the transmission number is retained at less than 1 throughout by NPIs, the number of cases will be less following relaxation.
However, the researchers suggest, “More realistic delivery scenarios may be simulated as vaccination deployment plans are better understood.”
In the increasing phase of the pandemic, the competition between the pace of vaccination and viral transmission indicates rapid indiscriminate vaccination rather than slower targeted campaigns. Thus, ordering is not essential when the vaccine delivery is either very fast or very slow, since in these situations, the number of new infections is negligible or the epidemic is complete, respectively, before vaccine delivery is completed.
Age-Dependent Efficacy
The effectiveness of vaccination varies, from a high below 45 years through a steady decline to a low at 85 years. This confirms the robustness of the early priority order, even with a low vaccine efficacy of just 20%.
At still lower efficacy levels, however, the first priority becomes people with underlying chronic illnesses or in the age group of 40-60 years. The researchers say, “The estimated number of deaths [is] relatively constant across a range of efficacy values for both older and younger age-groups.”
In fact, with the type 3 vaccine, up to efficacy of only 10%, the highest vaccine priority group continues to be the elderly.
Cost per Vaccine Dose
The researchers estimate that assuming a transmission number of 1.8, the loss of QALYs would be ~1.6 million if a second wave occurs. To prevent this, ~21 million targeted individuals must be vaccinated with ~41 million doses of vaccine, which is 90% effective. This suggests a per-dose cost of £767, in contrast to the cost-effective threshold of £20,000 per QALY, which is, by any standards, a huge benefit.
Implications and Future Directions
The conclusion is likely to hold good in all countries reflecting what is currently known about the virus: “It is important that the vaccine is deployed as efficiently as possible such that early limited supplies are used to greatest effect.”
Future research will incorporate other observed parameters as they become known, including the percentage of the population that will accept vaccination and the efficacy of the vaccine across age groups. The actual expected delay in vaccine deployment must also be included in model parameters.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources