The ongoing and disruptive COVID-19 pandemic, caused by the beta-coronavirus SARS-CoV-2, has shaken the world's healthcare systems and economy and claimed more than 2.22 million lives a year after its emergence.
Human adaptive immune system consists of cellular (T cell) and humoral (B cell) immunity and plays a crucial role in our defense against SARS-CoV-2. And while a coordinated interplay between the cellular and humoral arms seems to be indispensable for effective control, T cells appear to be capable of resolving the infection when B cell responses are deficient.
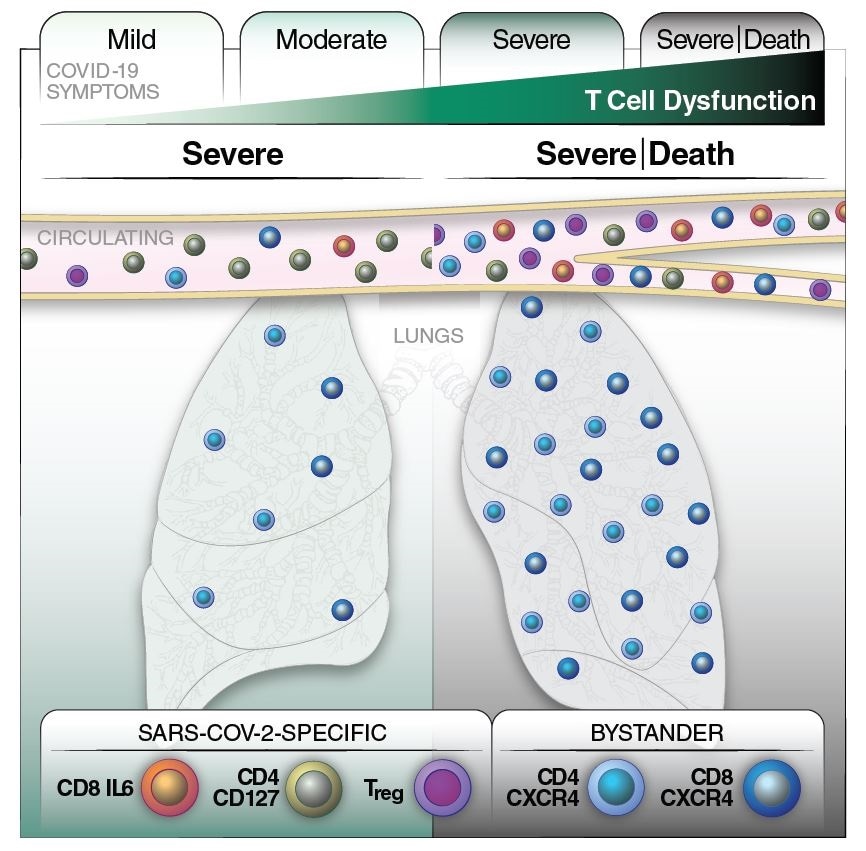
We know that a consistent feature of severe COVID-19 is T cell lymphopenia (i.e., an abnormally decreased level of lymphocytes in the blood), which is unlikely to merely indicate T cell sequestration in the infected lungs.
T cells as 'the most valuable players'?
T cells are likely key contributors to SARS-CoV-2 immunity; however, not much is known about the phenotypic features of SARS-CoV-2-specific T cells related to recovery from severe COVID-19. That said, some newer studies have analyzed the features of T cells recognizing SARS-CoV-2 epitopes.
Considering that these antigen-specific cells can recognize virally-infected cells and generate specific antibodies directly, they hold the most potential to show a beneficial effect on recovery from disease. They are also principal targets of vaccination endeavors.
In this study, a research group led by Dr. Jason Neidleman from the Gladstone Institutes and the University of California in San Francisco (USA) aimed to define the features of T cells from individuals hospitalized in the ICU due to COVID-19 – including some that successfully recovered and some that succumbed to the disease.
A deep phenotyping approach
In this study, the researchers have compared total and SARS CoV-2-specific T cells in mild, moderate and severe cases of COVID-19. Moreover, within the severe cases, an in-depth analysis of longitudinal specimens was conducted to pinpoint any predictive features linked to survival.
A total of 48 blood specimens from 34 individuals infected with SARS-CoV-2 have been analyzed, together with samples from 11 uninfected controls. Samples were taken from ICU patients classified as "severe cases" (68.8%), and from hospitalized patients without the need for the ICU, classified as "moderate cases" (31.2%).
The scientists implemented deep phenotyping of both total and SARS-CoV-2-specific T cells using 38-parameter CyTOF – a recently introduced technique for the characterization of T cells from convalescent individuals.
This enabled the identification of unique phenotypic characteristics of viral-specific and bystander T cells associated with recovery from severe disease, which was then paired with a comprehensive examination of the features of T cells present in the lungs of COVID-19 patients.
The role of SARS-CoV-2-specific T cells
Relative to patients who have died, individuals in this study that recovered from severe forms of COVID-19 presented with elevated numbers of SARS-CoV-2-specific T cells capable of honing a physiological response known as homeostatic proliferation.
More specifically, the researchers observed an increased number of CD8-positive transitional memory T-cells in patients with mild symptoms and a higher number of activated, PD1-expressing T-cells in patients with severe symptoms.
Conversely, in fatal cases of COVID-19, there was an elevated number of SARS-CoV-2-specific regulatory T cells and a time-dependent upsurge in activated bystander CXCR4+ T-cells (the latter subset of cells is also regarded as "extrafollicular" helper T cells).
When all results are taken into account, this study represents a model in which lung-homing T cells activated via bystander effect contribute to immunopathology, whereas a non-suppressive and robust SARS-CoV-2-specific T cell response controls pathogenesis and stimulates recovery from severe COVID-19.
Implications for vaccination efforts
In a nutshell, this study's findings support a favorable rather than immunopathologic role for effector SARS-CoV-2-specific T cells during the severe acute infection, together with promoting recovery from COVID-19.
"Taking into consideration the longevity of SARS-CoV-2-specific T cells, our results suggest that strategies to boost the effector functions of SARS-CoV-2-specific T cells, including by vaccination, will be beneficial for decreasing COVID-19 mortality and helping to end this devastating pandemic", say the authors of this medRxiv study.
In any case, since this study was correlative and phenotypical in nature, follow-up functional assays will be needed to establish any causal effect, as well as studies on larger cohorts of infected individuals.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references:
- Preliminary scientific report.
Prior to Peer Review Preprint - Neidleman, J. et al. (2021). Distinctive features of SARS-CoV-2-specific T cells predict recovery from severe COVID-19. medRxiv. https://doi.org/10.1101/2021.01.22.21250054, https://www.medrxiv.org/content/10.1101/2021.01.22.21250054v1
- Peer reviewed and published scientific report.
Neidleman, Jason, Xiaoyu Luo, Ashley F. George, Matthew McGregor, Junkai Yang, Cassandra Yun, Victoria Murray, et al. 2021. “Distinctive Features of SARS-CoV-2-Specific T Cells Predict Recovery from Severe COVID-19.” Cell Reports 36 (3). https://doi.org/10.1016/j.celrep.2021.109414. https://www.cell.com/cell-reports/fulltext/S2211-1247(21)00827-5.