As the coronavirus disease (COVID-19) continues to spread, it is speculated that it is also a vascular disease. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) affects the body beyond the respiratory tract, leading to various symptoms and complications.
Researchers at Tel Aviv University sought to identify how specific SARS-CoV-2 proteins affect the vasculature. They found that 70 percent of SARS-CoV-2 proteins affect vascular permeability, specifically targeting endothelial cells.
The study, published on the pre-print server medRxiv*, can pinpoint and isolate how each of the SARS-CoV-2 proteins independently affects the endothelial response and directly gauge endothelial functionality.
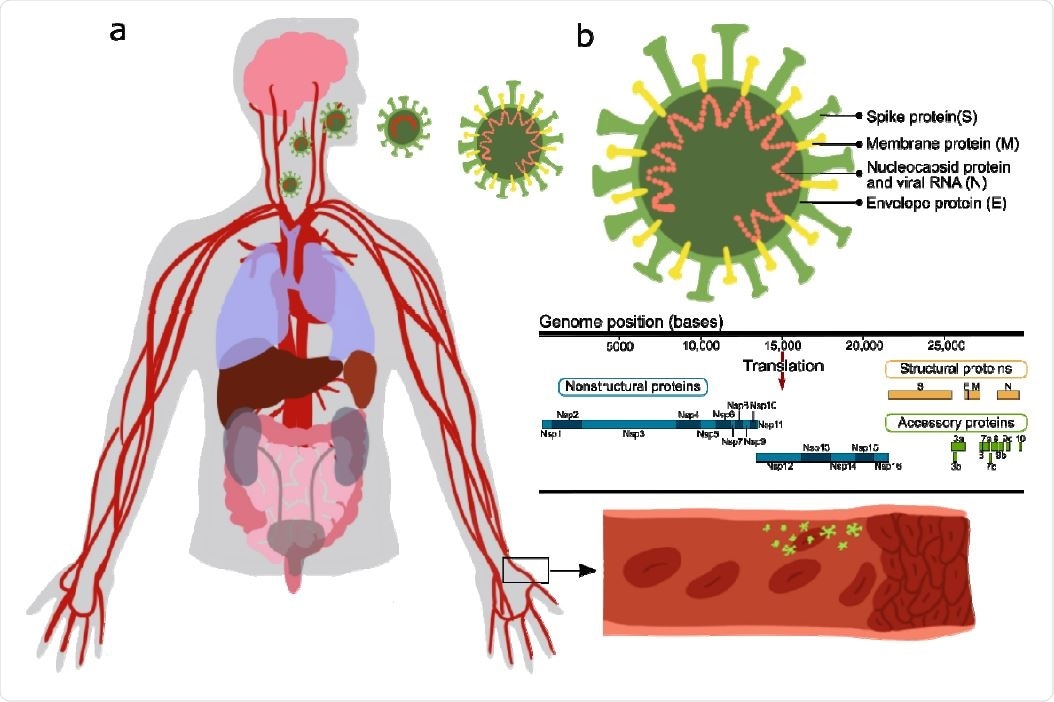
Effect of SARS-CoV-2 proteins on endothelial cells. a Sketch representing the main organs affected by SARS-CoV-2; b structure and gene composition of SARS-CoV-2.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
SARS-CoV-2 and the vascular system
The COVID-19 leads to severe disease in high-risk populations like the elderly and those with comorbidities. Often, severe disease is associated with cytokine storm, vascular dysfunction, progressive lung damage, and coagulation.
SARS-CoV-2 affects several vital organs, such as the lungs, heart, kidneys, and blood vessels, via its pathological effect on endothelial cells.
In a previous study, COVID-19 may cause severe disease. After the initial viral infection phase, about 30 percent of 40 patients hospitalized develop severe illness, with progressive lung damage and severe immune response. Consequently, other complications were observed, including low oxygen in the blood and cytokine storm. These led to heart and kidney failure.
Many of these pathologies were linked to the increased coagulation and vascular dysfunction. It is believed that aside from being a respiratory illness, COVID-19 may also be a vascular disease. It causes a leaky vascular barrier and heightened expression of von Willebrand factor (VWF), responsible for increased coagulation, inflammation, and cytokine release.
The alteration of the endothelial barrier in the blood vessels may be due to several factors. First, it could be the result of a direct effect on the endothelial cells, causing endothelitis and endothelial dysfunction. Second, it could be due to lysis and the death of endothelial cells.
Third, it could be due to sequestering of the human angiotensin-converting enzyme 2 (hACE2) by viral proteins that stimulate the kallikrein-bradykinin renin-angiotensin pathways, promoting vascular permeability.
Lastly, the overreaction of the immune system, wherein a combination of immune cells and neutrophils happens. This causes the production of reactive oxygen species, inflammatory cytokines, and vasoactive molecules.
Further, deposition of hyaluronic acid causes altered endothelial junctions, increasing vascular permeability, leakage, and coagulation.
The study
The SARS-CoV-2 genome encodes 29 proteins, contributing to the disease signs and symptoms, and endothelial complications are unknown.
To see the effects of these proteins on endothelial cells, the team cloned and expressed 26 of these proteins in human cells, particularly human umbilical vein endothelial cells (HUVEC). They observed the endothelial response to overexpression of each protein.
The team found that 70 percent of these proteins stimulated significant changes in endothelial permeability. Specifically, proteins nsp2, nsp5_c145a (catalytic dead mutant of nsp5), and nsp7 reduced CD31, called platelet endothelial cell adhesion molecule 1 (PECAM-1), which thought to be a sensitive and specific marker for vascular differentiation. They also increased von Willebrand factor expression and interleukin-6 (IL-6), suggesting endothelial dysfunction.
Further, the team applied their protein-protein interaction (PPI) network analysis and predicted the endothelial proteins affected by viral proteins. They used the PPI model to determine the role of each protein in other tissues affected by SARS-CoV-2.
Overall, the study identified which of the viral proteins are most dominant in affecting the virus's physiological response. The team believes that the study will provide a better insight into the mechanisms by which the vascular system responds to SARS-CoV-2 infection. From there, the team recommends that the findings may serve as a basis for drug development to target the identified proteins.
Finding an effective drug is essential as the virus has spread to 192 countries and regions, infecting over 114 million people. The virus has claimed 2.54 million lives globally.
Countries with the highest number of cases include the United States, with 28.71 million cases; India, 11.12 million cases; and Brazil, with 10.64 million cases.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Source:
Journal references:
- Preliminary scientific report.
Rauti, R., Shahoha, M., Leichtmann-Bardoogo, Y. et al. (2021). Effect of SARS-CoV-2 proteins on vascular permeability. medRxiv. https://www.biorxiv.org/content/10.1101/2021.02.27.433186v1
- Peer reviewed and published scientific report.
Rauti, Rossana, Meishar Shahoha, Yael Leichtmann-Bardoogo, Rami Nasser, Eyal Paz, Rina Tamir, Victoria Miller, et al. 2021. “Effect of SARS-CoV-2 Proteins on Vascular Permeability.” Edited by Arduino A Mangoni, Matthias Barton, Francesco Pasqualini, and Gad Vatine. ELife 10 (October): e69314. https://doi.org/10.7554/eLife.69314. https://elifesciences.org/articles/69314.