Children exposed to traffic-related air pollution show seasonal changes in their nasal bacteria, with winter pollution driving a shift toward less diverse, and potentially more harmful, microbial communities.
 Study: Short-term personal exposure to multiple air pollutants affects nasal microbiota in school-age children. Image Credit: khunkornStudio / Shutterstock
Study: Short-term personal exposure to multiple air pollutants affects nasal microbiota in school-age children. Image Credit: khunkornStudio / Shutterstock
Respiratory diseases are common in school-age children and are worsened by air pollution. Pollution-induced changes in the nasal microbiome may mediate this. A recent paper in the journal Science of the Total Environment reports that the nasal microbiota in children varies seasonally and is driven by two distinct types of air pollutants.
Introduction
Children living in cities are more vulnerable to air pollution because their immune and respiratory systems are still immature. Moreover, urban air often contains high levels of pollutants, which account for increased rates of asthma, pneumonia, poor lung function, allergic disorders, and respiratory infections.
Changes in the upper respiratory tract microbiota can reduce resistance to pathogens, promoting infection. Air pollution predisposes to such changes.
Earlier studies used proxy data rather than personal exposure to air pollution or focused on a single pollutant rather than a mixture of pollutants. They ignored seasonal shifts in respiratory microbiota, which may influence how they react to pollution. These shifts are caused by changes in the diet and in circulating viruses.
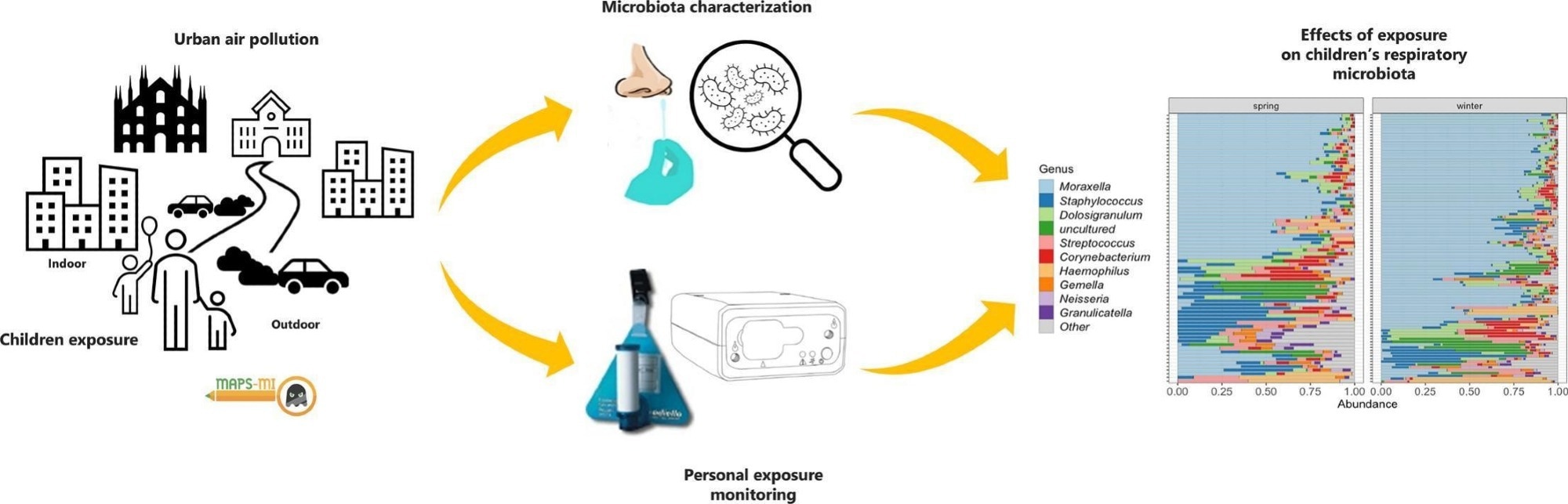
The current study addressed these factors together. The data came from the “MAPS MI” projects, which involved both parents and children in monitoring their exposure to air pollution over two seasons.
The study took place in Milan, Italy, in the spring and winter of 2018-2019. It captured exposures occurring during the usual routine of the children’s school-going year, including seasonal changes. The average age of the children was 8-9 years. About one in three children had pets, and a similar proportion were exposed to smoking at home.
The researchers fitted children with devices measuring equivalent Black Carbon (eBC) and volatile organic compounds (VOC). These represent particulate and gaseous pollutants, respectively. The devices collected data from the end of the school day to the beginning of the next school day. Nasal samples were also taken.
Study findings
All pollutants detected here were 2-3 times more concentrated in winter compared to spring. Of the 169 nasal samples, 95 and 74 were from winter and spring, respectively. Seasonal variation accounted for 3% of the difference in microbiota diversity between samples.
Winter samples showed an enrichment of Moraxella, while Staphylococcus was more enriched in spring. Moraxella tends to dominate other bacteria, reducing microbial diversity. This agrees with the reduced number of species found in winter.
This is perhaps because children spend more time indoors in less ventilated spaces and are not exposed to as many environmental microbes as they are in warmer seasons.
While Moraxella commonly inhabits children's airways, it can cause disease and worsen the symptoms of chronic disease or respiratory infection.
Peak eBC exposure reduced microbial diversity both in spring and winter, though the latter was not statistically significant. However, average eBC levels were more important than peak levels in their effects on the abundance of microbial genera. eBC could come from diesel exhaust, for instance, indicating that very short periods of exposure can produce hyper-responsive airways and worsen asthma attacks.
VOC exposure did not produce such consistent effects.
Certain species, like Corynebacterium, became less abundant with increasing air pollution. While the direction of this effect was generally consistent across seasons, for some exposures like peak eBC, the impact was more pronounced in spring. Others, like Neisseriaceae, became more abundant with increasing pollution, especially in spring. Species like Alloprevotella and Gemella showed pronounced seasonal shifts in their response to pollution levels; for example, exposure to benzene was associated with a decrease in their abundance in winter but an increase in spring.
VOCs produced the most obvious effects on the abundance of various genera, in contrast to the subtler effects of eBC. VOCs caused the Veillonella genus to become less abundant. For instance, methyl tert-butyl ether (MTBE) increased Neisseriaceae abundance, while limonene (often found in cleaning products) reduced it. Both benzene (a VOC) and eBC led to an increase in Moraxella abundance.
Phyla like Actinobacteriota and Fusobacteriota were decreased by limonene exposure.
Thus, air pollution reduces beneficial bacteria like Corynebacterium or increases potentially pathogenic species like Moraxella. Some species show a seasonal shift.
This knowledge should stimulate parents to improve indoor air quality. They should avoid indoor smoking, lighting scented candles or indoor fireplaces, and using cleaning products that release VOCs is one step.
To reduce peak exposures, children should use less busy routes to school. Policies should focus on creating low-pollution zones in and around schools.
Conclusions
The current study is the first to show how gaseous and particulate air pollution alter nasal microbiota in school-age children, and the importance of seasonal variation in its effects. Air pollutant exposure is 2-3 times higher in winter, and Moraxella is a dominant feature of the nasal microbiota, which shows reduced diversity.
Spring reduced air pollution levels, while the microbiota became more diverse. Staphylococcus became more abundant, this being a marker of other beneficial bacteria in the airway. This might indicate a more balanced composition of bacterial species in spring.
Air pollution causes inflammation and oxidative stress, which could alter the interactions between respiratory microbiota and the immune system and promote an increase in less abundant species at the expense of more common bacteria.
The authors acknowledge certain limitations, such as the relatively small sample size and the study's focus on children in a specific urban environment (Milan, Italy), which may affect the generalizability of the findings to other populations or settings. Reducing air pollution helps keep the respiratory microbiome more diverse, allowing beneficial commensals to dominate and reducing respiratory infection risk.