In a new experiment, scientists used virtual reality to show that the brain can sense virtual infection to trigger the body’s immune system, before the first microbe ever makes contact.
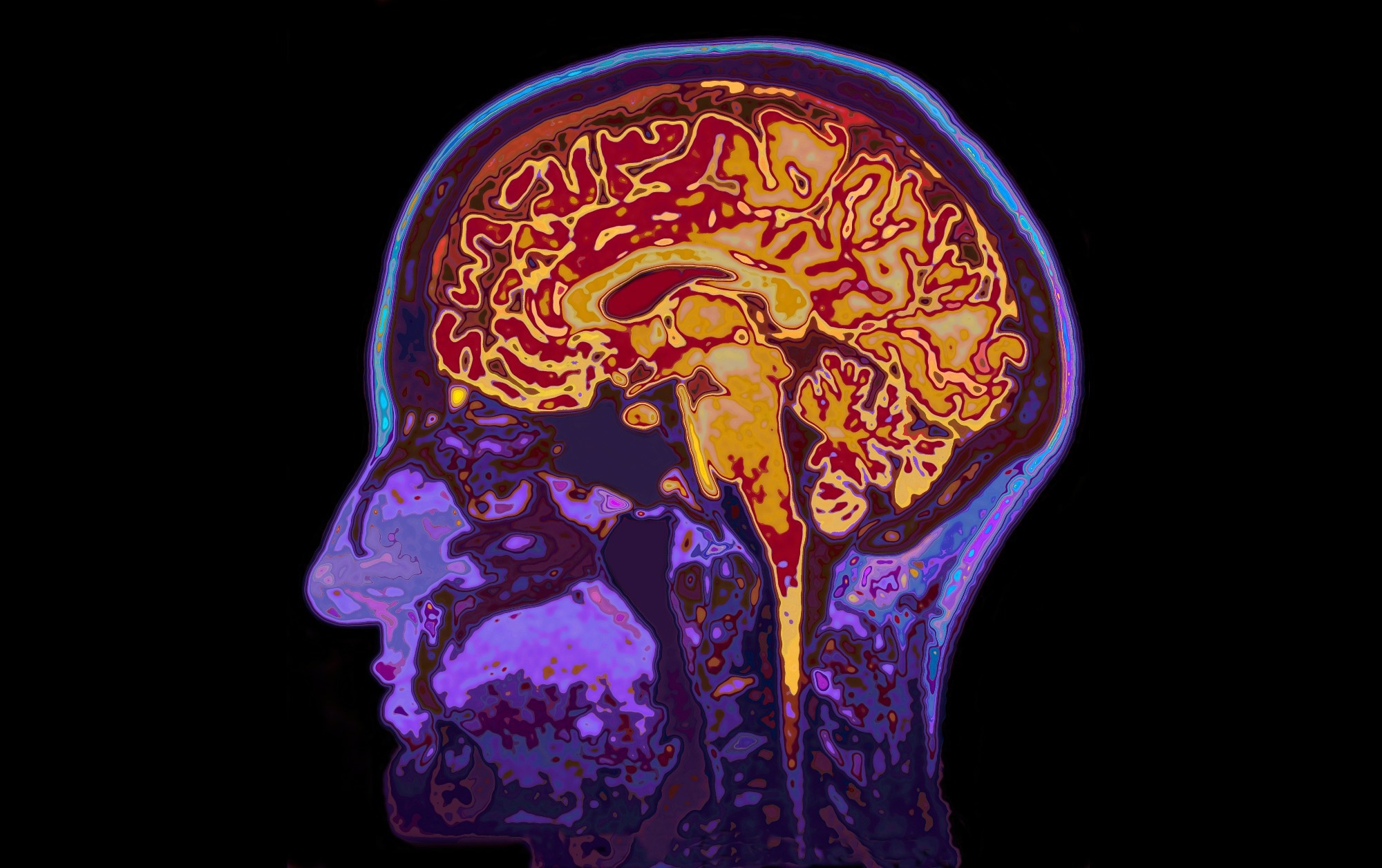 Study: Neural anticipation of virtual infection triggers an immune response. Image credit: SpeedKingz/Shutterstock.com
Study: Neural anticipation of virtual infection triggers an immune response. Image credit: SpeedKingz/Shutterstock.com
The immune system detects and responds to the presence of a pathogen to eliminate or counteract its toxic effects. However, the delay in this process might weaken its efficacy. A recent report in Nature Neuroscience shows how the neural system primes the immune response in anticipation of a potential infectious threat, even without actual pathogen exposure.
Introduction
Living organisms must be able to anticipate threats and respond immediately through a fight-or-flight reaction. Such mechanisms have been studied extensively, as they produce responses like social distancing that reduce the odds of spreading infection.
Primates have a neural network within the frontal and parietal neurons that integrates touch-mediated stimuli and data from external sensory receptors to sense stimuli in the peripersonal space. The immune system reacts to the stimulus via its innate and adaptive arms, triggering early and late immune responses. These ensure that pathogens are efficiently cleared without compromising host integrity.
Both neural and immune systems interact for mutual regulation. However, nothing shows that both systems respond in a coordinated manner to potential infections before contact with the infectious agent. The new study provides evidence of an anticipatory neuro-immune mechanism activated by potential infection threats before physical contact occurs.
The current study explored whether the human brain could anticipate virtual infections, triggering early immune responses, just as following physical contact with a pathogen.
About the study
The researchers used a virtual reality (VR) system to demonstrate neural circuits' anticipatory response to infectious entities within the peripersonal space.
The study comprised healthy participants who were first exposed to neutral avatars.
They were randomly assigned to one of three equal cohorts in the second session. Each cohort was exposed to a neutral, fearful, or infection virtual reality (VR) avatar.
The infection avatar implied potential infections, such as human face avatars with clear signs of infection, that entered the participants’ peripersonal space. These aroused avoidance responses to their perceived contagious nature. Since disgust is key to avoidance responses, cohorts were matched for disgust and anxiety thresholds. Disgust sensitivity was also included as a covariate in neuroimaging analyses to ensure it did not confound the effects of infection cues.
The researchers measured neural, behavioral, and immune responses to multisensory VR challenges using multiple modalities, including psychophysics, electroencephalography, and functional magnetic resonance imaging. For instance, reactions to tactile stimuli on the face were timed even as immersive VR showed an approaching avatar face, at five distances. This was normalized using the same stimuli but without any avatar to measure unisensory stimulation.
The distance at which the avatar produced a multisensory effect was determined: the peripersonal space effect (PPS effect). They compared the responses to the infection avatars with the reactions to controls, neutral and fear-inducing avatars, or to actual contact with a pathogen (by the injection of a flu vaccine).
Study findings
The type of avatar determined the change in the PPS effect from baseline to the second session. The PPS effect occurred at all distances with the infection avatar, vs. only the two closest distances at baseline. This indicates its anticipatory nature, induced before actual body-pathogen contact.
The results showed that the early response to potential infection occurred in multisensory-motor areas, such as the fronto-parietal brain areas that sense peripersonal space invasion. These predict potential infection in the close proximity of an infectious agent, leading to the activation of the salience network.
Importantly, this anticipatory brain response was specific to infectious avatars and did not occur with fearful avatars, demonstrating that the neural system distinguishes between pathogenic and generic threats.
The salience network is a cluster of connected brain regions designed to detect and select the most relevant stimuli. This results in the release of neuro-immune mediators in a sequence amplified at each step.
“Here, we show that the PPS network and the salience network respond to virtual infections to implement fast responses. Importantly, this pattern of brain activations was specific to detection of virtual infection.”
In response, behavioral changes occurred via altered connectivity in a network of areas, including the hypothalamus. The hypothalamus regulates innate immune responses through the hypothalamic-pituitary-adrenal cortex (HPA) axis, a key component of the neuro-immune interface.
Activation of the neuro-immune axis led to directed activation of the innate lymphoid cells and reduced frequency of these cells. This suggests their migration into the tissues. NK cells did not show significant changes, however.
“These data show that ILCs (innate lymphoid cells) react to infections not only when they are detected in the body but also when they are processed as a potential threat approaching the body.”
Using neural network models, scientists found that ILC activation was best predicted by a nonlinear interaction between three classes of mediators: HPA-related hormones, eicosanoids, and neuroinflammatory factors. Lymphoid cell activation corresponded almost linearly to HPA-related hormone levels, and the inverse was true of neuroinflammatory chemicals.
The strongest predicted immune response occurred in a “hot spot” of high HPA-related hormone levels, low levels of neuroinflammatory mediators, and intermediate eicosanoid concentrations. Actual data from the infection cohort were more likely to fall within this predicted range than the control group.
These suggest that “a virtual infection threat (and not a generic threat) induces a specific pattern of neuro–immune signaling, which is sufficient to drive ILC activation.”
Conclusion
The results of this experiment suggest that the neural and immune systems act in unison to anticipate threatened infection even without physical contact. Crossing the functional boundary of the peripersonal space leads to the detection of impending infection. This triggers anticipatory neural and immune activity.
The PPS system and salience network coordinate to recognize and respond to threats. This induces immune responses before actual infection via innate lymphoid cell activation. The HPA axis is probably involved in this response via neuro-immune cross-talk.
“Although surprising, our finding that immune responses can be triggered by simulated infections presented in VR is consistent with the principle of the smoke detector in biological systems.” The study also emphasizes the high sensitivity of the behavioral immune system to even false-positive stimuli, in this case delivered by VR.
The researchers caution that further studies are needed to validate the generalizability of these findings across age groups, stimulation types (e.g., looming vs. static), and other immune markers. However, the study introduces a new approach for investigating the anticipatory interface between perception, cognition, and immunity.
Future studies should clarify the differences in response to different stimulation types, namely looming vs. static stimuli, while validating the immune responses to virtual brain stimulation in humans.
Download your PDF copy now!