In a global trial of over 2,500 patients, obicetrapib dramatically reduced LDL cholesterol levels when added to standard lipid-lowering therapy, offering new hope for those at highest cardiovascular risk.
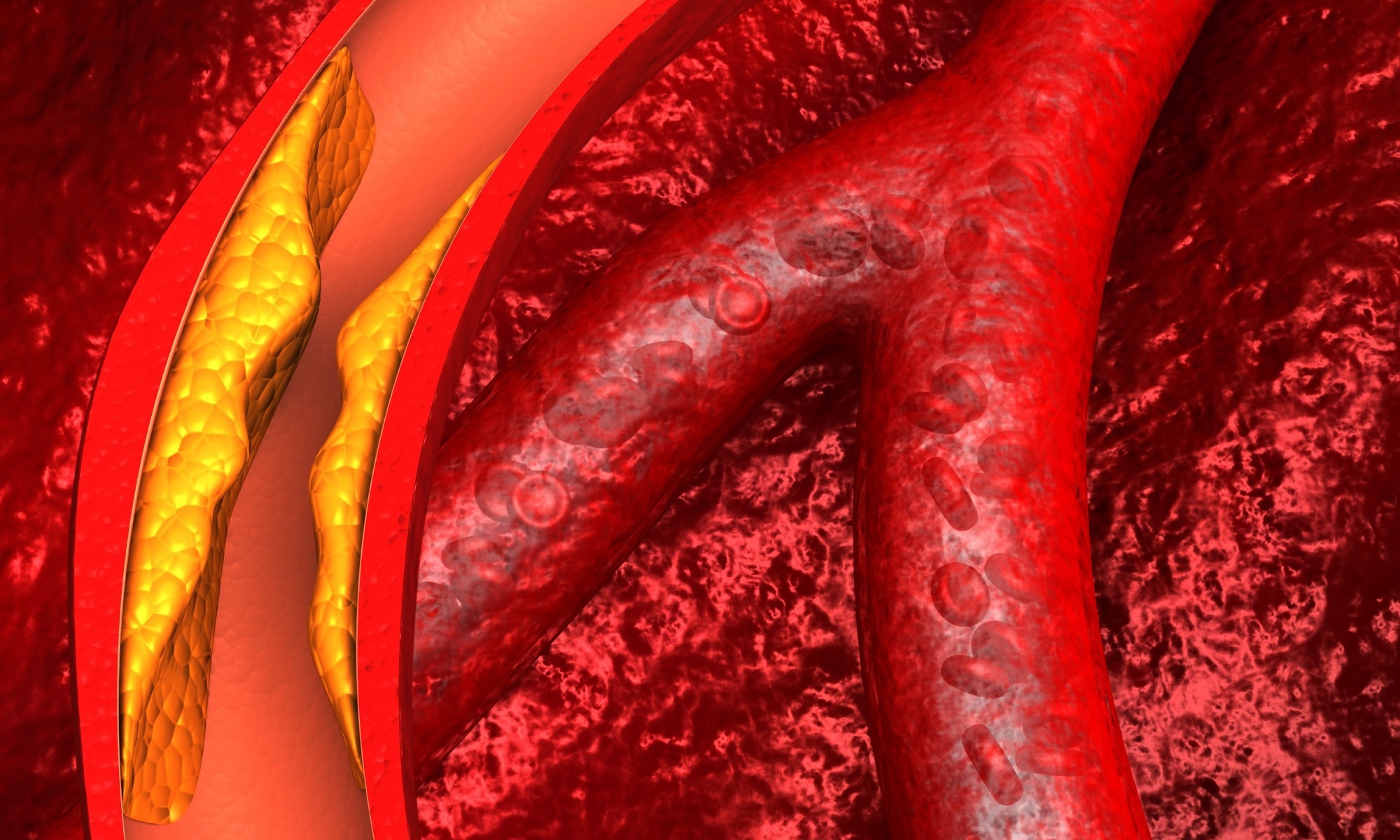 Study: Safety and Efficacy of Obicetrapib in Patients at High Cardiovascular Risk. Image Credit: Explode / Shutterstock
Study: Safety and Efficacy of Obicetrapib in Patients at High Cardiovascular Risk. Image Credit: Explode / Shutterstock
A recent New England Journal of Medicine study investigated the efficacy and safety of obicetrapib among patients at high risk of cardiovascular events.
Clinical benefits of LDL-lowering drugs and the context of CETP Inhibition
Multiple clinical trials have shown that lowering LDL cholesterol levels decreases the risk of cardiovascular events. The class of drugs known as cholesteryl ester transfer protein (CETP) inhibitors, to which obicetrapib belongs, has been explored for its potential to modify cholesterol levels. However, the development of CETP inhibitors has faced significant challenges; for instance, torcetrapib was associated with increased cardiovascular morbidity and mortality, and other agents like dalcetrapib and evacetrapib were discontinued due to a lack of efficacy in improving cardiovascular outcomes.
These past experiences have guided the development of newer agents like obicetrapib, which has a hydrophilic design intended to avoid some off-target effects and focuses on robust LDL cholesterol reduction in addition to raising HDL cholesterol. Low-intensity or high-intensity statin therapy focuses on lowering LDL cholesterol.
Combination therapy can help lower LDL cholesterol levels in patients at very high risk of cardiovascular events. However, the usage of combination lipid-lowering therapy is low, as evidenced by observational studies, which implies that more high-risk patients will receive inadequate treatment and potentially experience adverse cardiovascular outcomes.
Early trials have shown that obicetrapib lowers LDL cholesterol levels and raises high-density lipoprotein (HDL) cholesterol levels. When added to a maximum tolerated dose of lipid-lowering therapy, it can also help high-risk patients achieve LDL cholesterol treatment goals. Besides studying the effect of obicetrapib on lipid levels, examining its side effects and safety profile among patients at high risk of cardiovascular events is essential.
About the study
This study conducted a randomized, multinational, placebo-controlled trial with individuals aged 18 years or above. Participants had to have a history of atherosclerotic cardiovascular disease or heterozygous familial hypercholesterolemia and be on maximum tolerated doses of lipid-lowering therapy. Genotyping or clinical criteria were used to diagnose heterozygous familial hypercholesterolemia.
Patients were eligible if they had an LDL cholesterol level of 100 mg per deciliter or higher or a non-high-density lipoprotein (HDL) cholesterol level of 130 mg per deciliter or higher. Alternatively, individuals with an LDL cholesterol level of 55 to 100 mg per deciliter or a non-HDL cholesterol level of 85 to 130 mg per deciliter were also eligible if they had at least one additional cardiovascular risk factor.
Two groups were created, and participants were assigned to them randomly in a 2:1 ratio. The groups received either 10 mg of obicetrapib once daily or a matching placebo for 365 days. The percentage change in LDL from baseline to day 84 formed the primary endpoint. There were secondary endpoints as well, namely, the levels of non-HDL cholesterol, apolipoprotein B, triglycerides, and total cholesterol at days 84, 180, and 365, the percent change in LDL levels at days 30, 180, 270, and 365, and levels of apolipoprotein A1 and lipoprotein(a) at day 84.
Study findings
From December 2021 through August 2023, across multiple sites in China, Europe, Japan, and the United States, 2530 patients were randomly assigned to receive obicetrapib or placebo, of which 292 discontinued prematurely. The average age was 65 years, the average body mass index (BMI) was 29, and 34% were women. A total of 89% had atherosclerotic cardiovascular disease, 38% had diabetes, and 17% reported heterozygous familial hypercholesterolemia. Seventy percent were receiving high-intensity statins, while 27% were on ezetimibe. PCSK9 inhibitors were being administered to 4% of patients. At baseline, the average LDL and HDL levels were 98 mg per decilitre and 49 mg per decilitre, respectively.
The primary endpoints for patients receiving obicetrapib and placebo were estimated at −29.9% and 2.7%, respectively. A difference between groups of −32.6 percentage points was observed. At day 84, approximately 27.9% and 1.1% of patients in the obicetrapib and placebo groups exhibited LDL cholesterol levels below 40 mg per decilitre. Similarly, 51.0% and 8.0% of patients in the obicetrapib and placebo groups exhibited LDL cholesterol levels less than 55 mg per decilitre. The percentage of patients with LDL cholesterol levels below 70 mg per deciliter was 68.4% and 27.5% in the obicetrapib and placebo groups, respectively.
A secondary endpoint favored obicetrapib over placebo. A between-group difference at day 30 reduced the LDL cholesterol level by 36.6%, day 180 by 32.7%, day 270 by 30.2%, and day 365 by 24.0%. The study noted that the LDL cholesterol-lowering effect appeared to diminish somewhat by day 365, which the authors suggested might be partly due to discontinuation of the drug. The current study also estimated between-group differences in the apolipoprotein B level to be −18.9 percentage points at day 84, −18.3 percentage points at day 180, and −13.8 percentage points at day 365. A similar trend of reduction in between-group differences was observed in the non-HDL cholesterol level (−29.4 percentage points at day 84), lipoprotein(a) level (−33.5 percentage points at day 84), and triglyceride level (−7.8 percentage points at day 84). Conversely, obicetrapib led to significant increases in HDL cholesterol level (136.3 percentage points difference at day 84) and total cholesterol level (17.7 percentage points difference at day 84).
During the trial period, adverse events were observed in 59.7% of the obicetrapib patients and 60.8% of candidates in the placebo group. However, there were no apparent differences in the rates or severity of adverse events between the groups.
The paper also reported on 'adverse events of special interest.' Liver-enzyme abnormalities (alanine or aspartate aminotransferase levels >3 times the upper limit of normal) occurred in 0.6% of obicetrapib patients versus 0.9% in placebo patients, and muscle enzyme abnormalities (creatine kinase >5 times the upper limit of normal) occurred in 0.3% versus 0.4%, respectively. Worsening kidney function (defined as a decrease from baseline of more than 25% in the estimated glomerular filtration rate) was noted in 6.8% of obicetrapib patients compared to 8.3% in the placebo group. New-onset diabetes or worsening of glycemic control occurred in 35.1% of patients in the obicetrapib group and in 40.0% in the placebo group. The most frequently reported adverse events overall included COVID-19, hypertension, and upper respiratory tract infections, with similar incidences between groups. In 4.2% and 5.2% of patients belonging to the obicetrapib and placebo groups, respectively, experienced cardiovascular events, such as deaths from coronary heart disease, nonfatal myocardial infarction, coronary revascularization, or stroke. No significant changes in ambulatory blood pressure measurements at baseline and at day 270 were observed.
Conclusions
The current study revealed that obicetrapib treatment could effectively reduce LDL cholesterol levels by a placebo-adjusted 32.6 percentage points at day 84, among patients with heterozygous familial hypercholesterolemia or atherosclerotic cardiovascular disease who are at high risk of cardiovascular events. In the future, more clinical studies are required to determine the efficacy of this agent in preventing atherosclerotic cardiovascular disease, and the paper notes that a large, long-term cardiovascular outcomes trial is currently underway.