A simple blood test could revolutionize early Alzheimer’s detection, offering a less invasive and highly accurate tool to identify people at risk before symptoms appear.
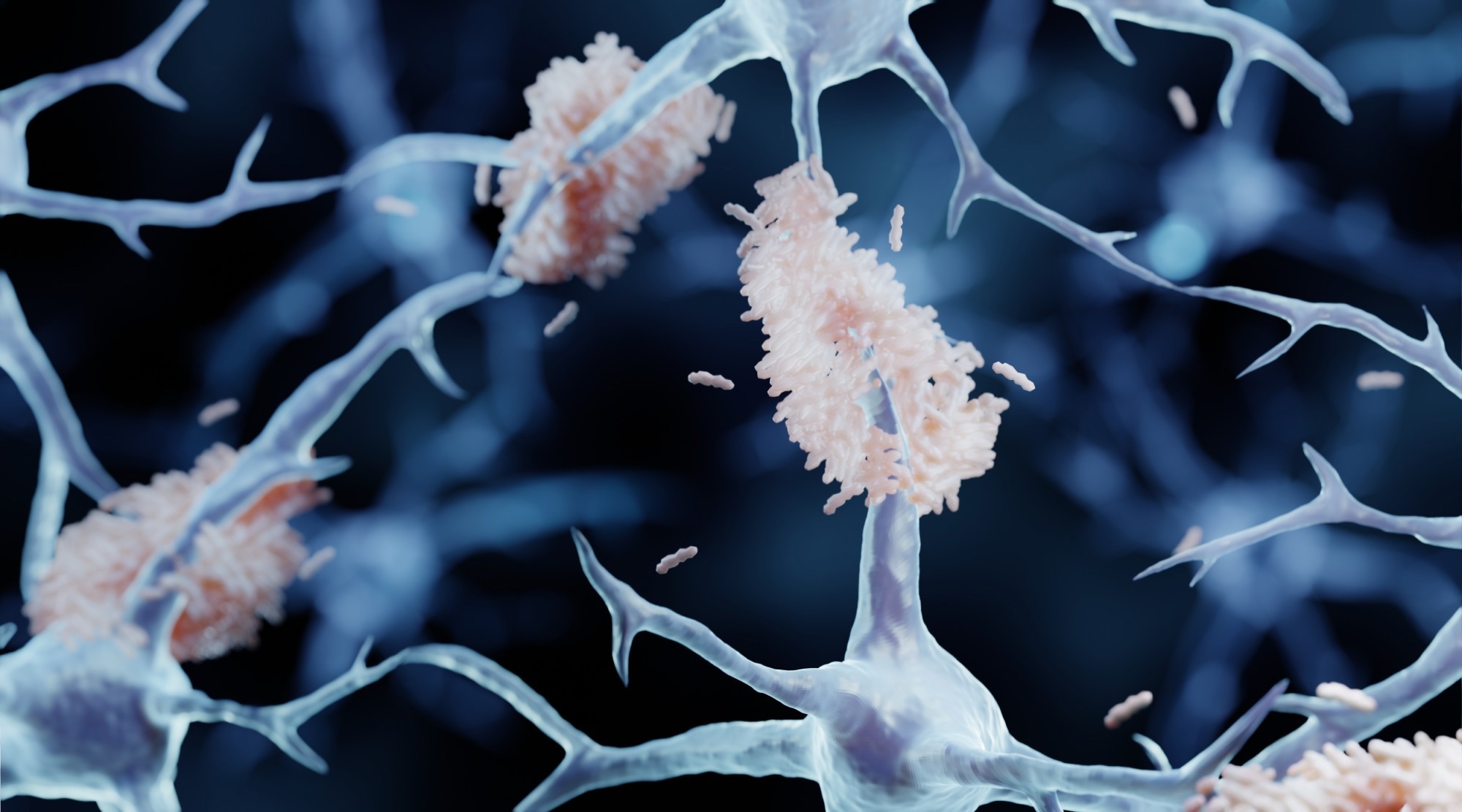 Study: A plasma biomarker panel for detecting early amyloid-β accumulation and its changes in middle-aged cognitively unimpaired individuals at risk for Alzheimer’s disease. Image Credit: ART-ur / Shutterstock
Study: A plasma biomarker panel for detecting early amyloid-β accumulation and its changes in middle-aged cognitively unimpaired individuals at risk for Alzheimer’s disease. Image Credit: ART-ur / Shutterstock
In a recent study published in the journal eBioMedicine, researchers evaluated the performance of plasma biomarkers to detect amyloid-β (Aβ) pathology in cognitively unimpaired (CU) individuals.
The preclinical stage of Alzheimer’s disease (AD) is a period when the accumulation of phosphorylated tau (p-tau) and Aβ begins to occur, but cognitive impairment is not yet evident. Accurate in vivo detection of this stage relies on core positron emission tomography (PET) and cerebrospinal fluid (CSF) biomarkers. Nonetheless, the low accessibility, high costs, and perceived invasiveness of these methods are significant obstacles.
On the other hand, blood-based biomarkers are a convenient and minimally invasive alternative. The most promising blood-based AD biomarkers include p-tau181, p-tau231, p-tau217, and Aβ42/40 ratio, among others. These biomarkers are significantly altered in response to growing Aβ burden, and their sensitivities and ability to detect group- or individual-level Aβ pathology vary.
About the study
In the present study, researchers evaluated the robustness and performance of various plasma biomarkers to detect Aβ pathology in CU individuals using a fully automated immunoassay platform. They included participants from the nested Alfa+ cohort within the Alzheimer’s and Families (ALFA) study, who had available baseline CSF and (at least one) plasma biomarker measurements. Alfa+ subjects were stratified based on CSF Aβ cutoffs. Participants were considered CSF Aβ-positive (A+) if their CSF Aβ42/40 ratio was < 0.071.
Subjects were also classified based on Aβ PET status, using a cutoff of 12 Centiloid. The primary cognitive outcome was a modified version of the Preclinical Alzheimer’s Cognitive Composite (mPACC). The Wilcoxon rank-sum test was used to compare demographics between Aβ groups. A type III analysis of covariance was performed to evaluate plasma biomarker differences between groups, calculating effect sizes like partial eta-squared (η²) to quantify the strength of these differences.
Further, multiple linear regression models assessed the associations between baseline plasma biomarkers and sex, age, body mass index (BMI), renal function, and apolipoprotein E (APOE) ε4 carrier status. Multiple linear regressions were used to assess associations between baseline plasma biomarkers and between baseline and three-year longitudinal changes in primary pathology, cognitive function, and neurodegeneration markers.
Further, the team investigated the relationship of longitudinal plasma biomarker changes with concurrent longitudinal changes in soluble tau and Aβ pathology, cognitive function, and neurodegeneration markers. All regression models were adjusted for sex, age, renal function, and BMI.
Findings
The study included 400 CU participants from the Alfa+ cohort. Of these, 33.8% were A+ based on the CSF Aβ42/40 ratio, and 66.2% were Aβ-negative (A-). Amyloid PET data were available for 342 participants, and only 15.8% were A+. Notably, there were significant differences in all plasma biomarkers between the A+ and A- groups, with plasma p-tau217/Aβ42 and p-tau217 showing the largest effect sizes (η² = 0.28 and 0.23, respectively).
Plasma glial fibrillary acidic protein (GFAP), neurofilament light (NfL), p-tau217/Aβ42 ratio, and p-tau217 increased with age, whereas plasma Aβ42/40 ratio decreased. Females had higher plasma GFAP; among APOE ε4 carriers, NfL and Aβ42/40 were lower, but plasma p-tau217, p-tau217/Aβ42, and p-tau181/Aβ42 were higher. Importantly, the plasma Aβ42/40 and p-tau217/Aβ42 ratios were not affected by renal function, a known confounder.
The team found that plasma Aβ42/40 (with an Area Under the Curve (AUC) of 0.86 for CSF Aβ status and 0.88 for PET Aβ status), p-tau217 (AUC = 0.80 for CSF Aβ status; AUC = 0.91 for PET Aβ status), p-tau217/Aβ42 (AUC = 0.85 for CSF Aβ status; AUC = 0.94 for PET Aβ status), and p-tau181/Aβ42 (AUC = 0.82 for CSF Aβ status; AUC = 0.90 for PET Aβ status) had the highest performance to detect A+ CU individuals. Plasma p-tau217/Aβ42 had the best performance for PET A+ (AUC = 0.94). However, the paper highlighted that the robustness of plasma Aβ42/40 was limited due to its sensitivity to analytical variability, potentially restricting its clinical utility despite its good discrimination accuracy. Plasma GFAP, NfL, and p-tau181 had lower overall performance individually, but their accuracy improved when combined with plasma ApoE4 (e.g., adding plasma ApoE4 significantly improved the discrimination of CSF Aβ status by plasma p-tau181 to an AUC of 0.80, and for plasma GFAP and NfL, AUCs for discriminating CSF and PET Aβ status ranged from 0.69 to 0.79 with ApoE4).
Furthermore, some biomarkers like plasma Aβ42/40, p-tau181/Aβ42, and p-tau217/Aβ42 showed associations with amyloid PET levels even in individuals classified as PET Aβ-negative, suggesting an early rise (or decrease for Aβ42/40) before the established onset of abnormal Aβ accumulation.
All baseline plasma biomarkers were associated with longitudinal increases in amyloid PET Centiloid.
Plasma Aβ42/40, p-tau217/Aβ42, and p-tau181/Aβ42 were associated with longitudinal reductions in CSF Aβ42/40, though the association for p-tau217/Aβ42 was noted after removing outliers. In addition, all baseline plasma biomarkers, except GFAP, were associated with longitudinal changes in CSF p-tau181. Furthermore, all plasma biomarkers at baseline were associated with longitudinal increases in CSF NfL, with some of these associations (e.g., for plasma Aβ42/40, p-tau181, and p-tau181/Aβ42) showing significance only after excluding outliers.
The increases in p-tau217 and p-tau217/Aβ42 were significantly associated with the longitudinal increase in Aβ burden. Longitudinal increases in plasma GFAP were associated with reductions in CSF Aβ42/40 and Aβ PET accumulation, with the latter association (Aβ PET accumulation) observed only in individuals who were initially PET Aβ-negative at baseline. Increases in plasma NfL were associated with decreases in CSF Aβ42/40. Notably, changes in plasma biomarkers were not associated with a longitudinal increase in cognitive changes, which the researchers suggested could be due to the relatively short follow-up of around three years and the early stage of the cohort.
Conclusions
The findings indicate that plasma p-tau217 and Aβ42/40, p-tau217/Aβ42, and p-tau181/Aβ42 ratios were the best-performing biomarkers in distinguishing A+ CU individuals from A- counterparts. Further, p-tau217/Aβ42 had the highest performance in detecting PET A+ subjects. However, the limited robustness of plasma Aβ42/40, as highlighted in the paper, needs to be considered for its clinical application. All plasma biomarkers at baseline were associated with longitudinal increases in PET Centiloid. It is also important to consider the study's limitations, such as its single-center design and a cohort enriched for AD risk factors, which may affect the generalizability of the results to other populations. Further studies with larger sample sizes, more diverse cohorts, and longer follow-up are necessary to corroborate and extend these results.