An international review uncovers the alarming rise in diabetes and related complications in youth, exposing urgent gaps in care and highlighting the need for bold preventative action.
 Study: Metabolic disorders in young people around the world. Image credit: Roman Chazov/Shutterstock.com
Study: Metabolic disorders in young people around the world. Image credit: Roman Chazov/Shutterstock.com
Scientists conducted a systematic review to evaluate the prevalence of metabolic diseases and the associated cardiometabolic complications among young adults. This review is published in Diabetologia.
Prevalence of metabolic diseases in youth
The increase in the global prevalence of metabolic diseases among youth has been attributed to rapid economic development, along with environmental and societal changes. Based on geographic locations, this increase is more significant in low- and middle-income countries (LMICs).
Obesity is a well-established risk factor for type 2 diabetes (T2D). In obese children, the hormonal changes in puberty can influence the shift from a metabolically healthy to unhealthy status. Obesity may also contribute to the earlier onset of type 1 diabetes (T1D) in genetically susceptible individuals. When it begins in youth, obesity is often accompanied by several cardiometabolic risk factors, including insulin resistance, hypertension, and increased risk of developing T2D. Additionally, risk-taking behaviors common in adolescence, such as smoking, alcohol use, and drug consumption, can further increase the risk of complications and reduce adherence to medical interventions.
The SEARCH for Diabetes in Youth study in the USA has reported that the incidence of T2D among youth has doubled between 2002 and 2018. Similar trends have been noted elsewhere, and in more recent data from the multinational SWEET registry, covering the period from 2012 to 2021. The highest and lowest growth rates were reported in North America and Europe, respectively. Rates in Asia, the Middle East, and Africa showed no statistically significant change.
Compared to T1D, the genetic background plays a more significant role in the development of T2D. However, obesity alone is not sufficient to cause T2D, as seen in Asian youth, where many cases occur despite lower rates of obesity. This suggests that genetic predisposition and environmental exposures contribute to disease risk. Additionally, early-life factors, such as the intrauterine environment, have increased the likelihood of developing T2D later in life. T2D also disproportionately affects marginalized and socioeconomically disadvantaged youth, with a large proportion of study participants living in poverty or under adverse social conditions.
Recent data shows that 19.8% of individuals living with T1D are under 20 years old. A cross-country systematic review documented an overall incidence rate of 14.07 per 100,000 person-years for those under 20 between 2000 and 2022. Incidence rates were lowest in Western sub-Saharan Africa and highest in Finland and high-income North America.
The higher rates in White populations can be attributed to specific genetic risk factors (i.e., HLA-DR3 and HLA-DR4 alleles). HLA-DR9 and HLA-DR7 have been associated with increased T1D susceptibility in Japanese and African American populations, respectively. In Asian populations, the presence of neutral or protective DQ alleles alongside risk alleles may continue to lower incidence rates.
Genetic alterations are not quick, and therefore, the rapid rise in T1D incidence could be driven by environmental determinants. The rapid rise in obesity could impact the incidence of T1D. Young people from lower socioeconomic backgrounds and racial and ethnic minority groups have shown higher T1D incidence. Socioeconomic disadvantage is also linked to reduced access to advanced care technologies, such as continuous glucose monitoring systems. Cost, training limitations, and availability also contribute to disparities in technology access.
Risks of complications and mortality in case of early-onset diabetes
Adolescents and children with T1D and T2D experience higher mortality and morbidity rates relative to the general population. Cardiovascular complications mainly drive this. Youth with T2D show more severe insulin resistance and rapid pancreatic beta cell function deterioration. Data from the SEARCH study has shown that youth with diabetes often show subclinical signs of vascular complications. These include background retinopathy, increased urinary albumin excretion, and cardiac autonomic dysfunction, even before symptoms appear.
The risk of complications is increased by factors such as hypertension, dyslipidemia, obesity, and insulin resistance. Relative to boys, girls experience higher HbA1c levels and BMI, more severe insulin resistance, and a greater prevalence of dyslipidemia during adolescence.
Lower levels of IGF-1 have been associated with the development of albuminuria in girls with T1D. Additionally, increased androgen levels have been linked to early signs of vascular damage in girls with albuminuria. These hormonal imbalances often include reduced sex hormone-binding globulin (SHBH) and elevated free androgen index.
Children diagnosed earlier in life face longer exposure to the effects of diabetes, which increases the risk and severity of complications over time. Youth with T1D from LMICs show a higher prevalence of vascular complications compared to those from high-income countries. Furthermore, the risk of complications is significantly influenced by ethnic disparities, even after adjusting for age and socioeconomic status.
Higher all-cause mortality has been associated with an earlier age at diagnosis of T2D, as evidenced by a meta-analysis of approximately 1.3 million individuals. A 1-year increase in age at diagnosis was associated with a 4% reduction in all-cause mortality, controlling for current age. The SEARCH study showed higher standardized mortality ratios for youth-onset T2D than T1D. Racial and ethnic minority groups exhibited the highest excess mortality.
Importantly, most deaths in youth with T2D were not due to diabetes itself, but to external causes such as injury or assault. In LMICs and low-income countries (LICs), life expectancy is markedly reduced due to acute and chronic complications such as infections, hypoglycemia, diabetic ketoacidosis, and end-stage renal failure.
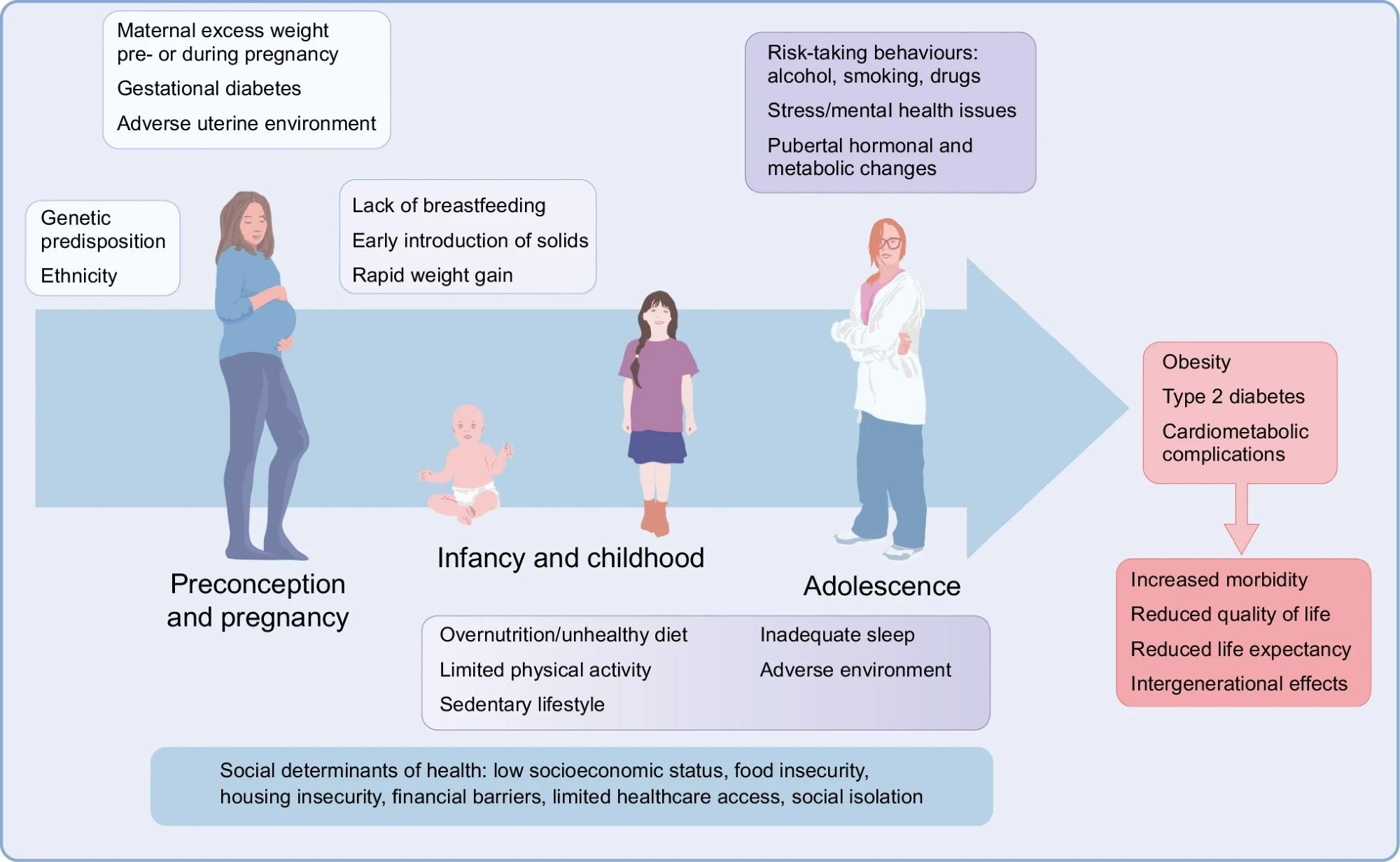 Life course of metabolic diseases in young people. The figure summarises the main risk factors acting during prenatal life, infancy, childhood and adolescence that contribute to the development of metabolic diseases, such as obesity and diabetes, as well as associated cardiometabolic complications.
Life course of metabolic diseases in young people. The figure summarises the main risk factors acting during prenatal life, infancy, childhood and adolescence that contribute to the development of metabolic diseases, such as obesity and diabetes, as well as associated cardiometabolic complications.
Solutions to curb early-onset metabolic diseases
To tackle the problem at hand, interventions should begin from pre-conception and continue through adolescence. Modifiable risk factors such as diet and physical activity should be focused on. A mix of lifestyle and behavioural interventions is needed to promote long-term health.
Regulation of food marketing and enhancement of nutritional labeling are essential to aiding youth in making informed choices concerning their food intake. Policy examples, such as taxation on sugar-sweetened beverages, have shown success in reducing obesity rates. Community-based initiatives and active school environments could make physical activity accessible and enjoyable. Clearer, evidence-based labelling and impartial access to healthier food options are also emphasized in the review.
Another critical step is raising awareness of metabolic diseases and their adverse health implications. Policies are required to overcome barriers to treatment adherence and mitigate therapeutic inertia, which is the reluctance to start or escalate necessary treatments. Healthcare providers may hesitate due to concerns over long-term safety data and lack of training, especially regarding newer treatments like GLP-1 receptor agonists. Clinical trials of new interventions in obese youth could be fast-tracked, as it is essential to expand treatment options. To develop targeted interventions, understanding ethnic and socioeconomic disparities across countries is important.
Concerning LMICs, the development of necessary infrastructure could significantly reduce the problem of delayed diagnosis and bring down treatment costs. Even scaling up to intermediate-level diabetes care, with basic insulin regimens, regular HbA1c testing, and age-appropriate education, has reduced mortality and is cost-effective in low-resource settings. The paper also highlights that such scaled care models are feasible and can meaningfully reduce the burden of complications when advanced therapies are unavailable.
Download your PDF copy now!