Radiotherapy is a common strategy employed for the battle against cancer, with around 50 percent of cancer patients receiving radiotherapy at some point during their treatment. It involves the application of ionizing radiation to the site of a tumor to destroy the cancer cells. Radiotherapy is generally considered the most effective means of reducing recurrence after surgical removal of a tumor.
In this case study, researchers used Electron Paramagnetic Resonance (EPR) spectroscopy to quantify radiation dose distribution perturbations.
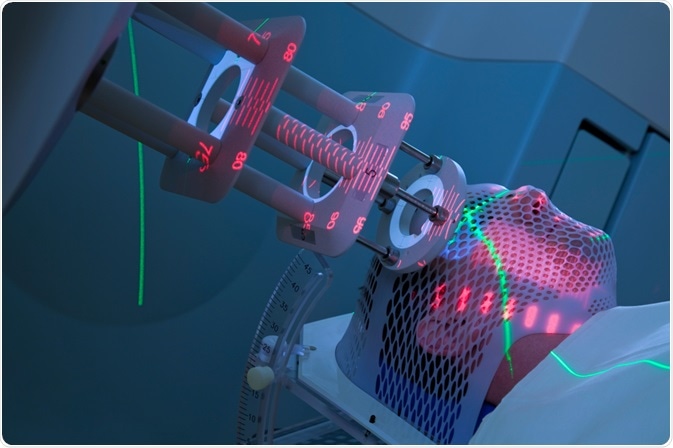 Image Credit: Mark_Kostich / Shutterstock.com
Image Credit: Mark_Kostich / Shutterstock.com
The radiation delivered during radiotherapy can damage healthy cells, which may cause adverse side effects. Consequently, radiographers aim to target the tumor with a destructive high dose of radiation whilst minimizing the amount of radiation that reaches the surrounding healthy cells1. To achieve this, accurate patient positioning and direction of the radiation beam are required, and these are usually confirmed using imaging techniques2.
Magnetic resonance imaging (MRI), with the benefits of not requiring further radiation exposure and providing superior soft tissue contrast, has been adopted as a preferred imaging modality for image-guided radiotherapy. Indeed, hybrid instrumentation that both delivers the therapeutic radiation and performs MRI scanning are available3.
However, the magnetic field used during MRI scanning can affect the amount of ionizing radiation reaching the target site and the extent of this effect has been difficult to quantify.
Effect of magnetic fields on radiation dose
The strong magnetic fields required for MRI can alter radiation dose distributions considerably4. The magnetic field can be applied either parallel or perpendicular to the radiation beam, but in both instances, the distribution of the radiation dose is disturbed as a result of the trajectory of released electrons being deflected by the magnetic field lines. The effect is especially significant at tissue-air interfaces due to the electron return effect (ERE)5.
The consequence can be dose enhancements and/or reductions at the target site. In addition, the reflected beam may increase the radiation exposure of, and so increase damage to, surrounding healthy tissue6. This is a concern, since it may reduce the efficacy of radiotherapy and increase the risk of side effects.
Thus, there is a need for the magnetic field induced perturbations of radiation dose distributions to be thoroughly investigated. However, quantifying the effect within a sub-millimeter thick surface layer has proved highly challenging.
Quantifying the effects of magnetic field on radiation dose
Numerous attempts to theoretically determine the precise nature of the radiation dose distribution perturbations have been made using simulation models7,8. Indeed, a toolkit capable of simulating particle transport through matter in the presence of external magnetic fields has been validated for medical physics applications.8 However, these are theoretical evaluations and experimental validation of the findings has remained elusive.
Radiochromic film and plastic have been used to evaluate relative dosimetry in the presence of strong magnetic fields, but such techniques have been hindered by several different kinds of artifacts that limit the maximum surface-to-volume ratio of such dosimeters and restrict the minimum analyzable detector size9.
Most recently, electron paramagnetic resonance (EPR) has been used to quantify the magnetic field induced perturbations of radiation dose distributions10. A 0.5 mm layer surrounding millimeter-sized air cavities was irradiated with a 6 MV photon beam in both the presence and absence of a transverse magnetic field.
The spatial distributions of radiation-induced paramagnetic defects were subsequently determined using a Bruker ELEXSYS E580 X-band EPR spectrometer in pulsed mode. The magnetic field gradient was generated in two planes using a Bruker E 540 GCX2 gradient coil system. The Bruker ER 4108 TMHS imaging resonator was used for echo detection.
Transverse magnetic fields were shown to result in local dose enhancements and reductions of up to 35%. The experimentally determined dose distributions were in good quantitative agreement with the values derived through theoretical simulations10.
This research demonstrates the feasibility of using EPR to measure magnetic field induced perturbations of dose distributions within a sub-millimeter thick surface layer at the dosimeter-air interface.
References
- Nutting C, et al. BJR 2000;73:459–469.
- Jaffray DA. Nature Reviews Clinical Oncology 2012;9:688–699.
- Raaymakers BW, et al. Phys. Med. Biol. 2017 ;62:23.
- Richter S, et al. Current Directions in Biomedical Engineering 2017;3:281.
- Raaijmakers AJE, et al. Phys. Med. Biol. 2005;50:1363
- Rubinstein AE, et al. PLOS ONE 2018;13:e0205803
- Oborn BM, et al. Medical Physics 2010;37:5208–5217
- Agostinelli S, et al. Spectrometers, Detectors and Associated Equipment 2003;506(3):250
- Costa F, et al. Phys. Med. Biol. 2018;63:05NT01
- Höfel S, et al. EPR imaging of magnetic field effects on radiation dose distributions around millimeter-size air cavities. Phys. Med. Biol. 2019. https://doi.org/10.1088/1361-6560/ab325b
About Bruker BioSpin Group
The Bruker BioSpin Group designs, manufactures, and distributes advanced scientific instruments based on magnetic resonance and preclinical imaging technologies. These include our industry-leading NMR and EPR spectrometers, as well as imaging systems utilizing MRI, PET, SPECT, CT, Optical and MPI modalities. The Group also offers integrated software solutions and automation tools to support digital transformation across research and quality control environments.
Bruker BioSpin’s customers in academic, government, industrial, and pharmaceutical sectors rely on these technologies to gain detailed insights into molecular structure, dynamics, and interactions. Our solutions play a key role in structural biology, drug discovery, disease research, metabolomics, and advanced materials analysis. Recent investments in lab automation, optical imaging, and contract research services further strengthen our ability to support evolving customer needs and enable scientific innovation.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.