Patients with malignant diseases often experience imbalances in serum electrolytes, which include hyponatremia, hypokalemia/hyperkalemia, hypercalcemia, and hypophosphatemia.
In many instances, the causes of such disturbances are joint etiologies that are not unique to certain cancer types. Nonetheless, these electrolyte imbalances may also signal the existence of paraneoplastic processes and foreshadow a dire prognosis.
Moreover, the development of electrolyte abnormalities is frequently associated with symptoms that negatively affect the quality of life and, in turn, prevent the action of certain chemotherapeutic agents.
Among the malignancies, lung cancer is considered to be the leading cause of cancer-related deaths around the globe. The two major types of lung cancer include small-cell lung cancer (SCLC) and non-small-cell lung cancer (NSCLC). The former condition is especially prone to give rise to electrolyte imbalances.
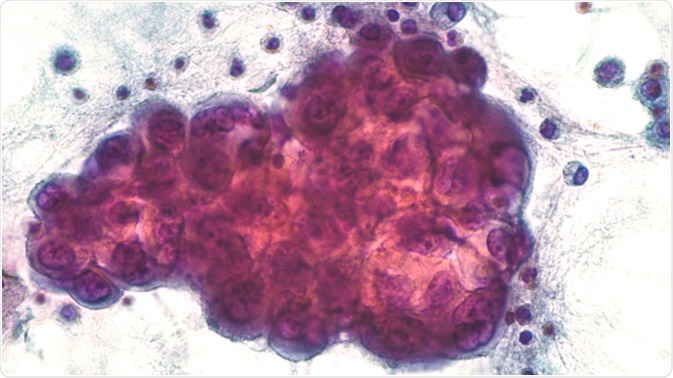
Malignant effusion: Pleural fluid pathology (cytology) of pulmonary adenocarcinoma, a type of NSCLC. Image Credit: David Litman / Shutterstock
Hyponatremia in lung cancer
Hyponatremia, otherwise known as low blood sodium levels, is the most common electrolyte imbalance disorder found in lung cancer patients. This condition can be related to a plethora of causes, including concurrent diseases, incidental medications, side effects of antineoplastic therapy regimens, or the disease itself.
Albeit not always life-threatening, hyponatremia is often associated with extended hospitalization, delays in scheduled chemotherapy, aggravated patient performance status, negative treatment response, diminished quality of life, and lower survival rates.
Hyponatremia is often seen in SCLC and is usually related to the syndrome of inadequate secretion of antidiuretic hormone (SIADH). It is basically a dilution example of low blood sodium linked to increased renal water retention. Conversely, only a handful of studies specifically focus on hyponatremia in NSCLC patients.
A recent study that examined the use of carboplatin in NSCLC found that this condition is significantly associated with the development of hyponatremia. The mechanism responsible for this association could be explained by uncontrolled water ingestion and decreased concentrations of serum electrolytes.
In any case, treatment of hyponatremia must be personalized and based on both the duration and severity of sodium serum reduction, underlying etiology, and extracellular fluid volume. All data that is currently available in the literature indicates that early correction of concentration levels is of the utmost importance.
The main options to achieve that goal are hypertonic or isotonic saline, fluid restriction, loop diuretics, urea, and tolvaptan, which is a vasopressin receptor 2 antagonist. For many patients with cancer-related SIADH, the hyponatremia can be refractory to therapy, thus other therapeutic avenues must be explored.
Dr. Rapoport Discusses Hyponatremia in Patients With Cancer
Other electrolyte disturbances in lung cancer patients
Hypokalemia is the second most frequent electrolyte imbalance seen in patients with malignant diseases. In SCLC, amongst the important causes of low potassium levels in the blood are adrenocorticotrophic hormone (ACTH)-secreting tumors.
Ectopic Cushing’s syndrome, secondary to lung cancer, is a rare occurrence with a poor prognosis but may manifest with severe hypokalemia, alongside hyperglycemia and muscle weakness. The proper control of severe hypercortisolism prior to administering systemic chemotherapy may result in prolonged survival.
Furthermore, squamous-cell carcinomas in the lung have been reported to result in hypercalcemia by means of parathyroid hormone-related protein (PTHrP) release. Although considerably less frequent, neoplasms of pulmonary origin can also make parathyroid hormone themselves.
Small molecular-targeted medical drugs that are increasingly being used may also exert adverse electrolyte reactions such as hypophosphatemia and hypomagnesemia. Therefore, attentive monitoring of phosphate and magnesium ions in the serum, which is still often neglected, represents a key issue in these cases.
In conclusion, it is well established in medical literature that electrolyte imbalances represent an additional risk factor for patients with malignancies. A prompt recognition of electrolyte imbalances and corrective therapy is pivotal when caring for patients presenting with lung cancer.
References
Further Reading
Last Updated: May 13, 2023