A new AI tool reads lung cancer biopsy slides in under an hour, accurately predicting mutations and saving patients delays, costs and tissue loss, marking a turning point in precision cancer care.
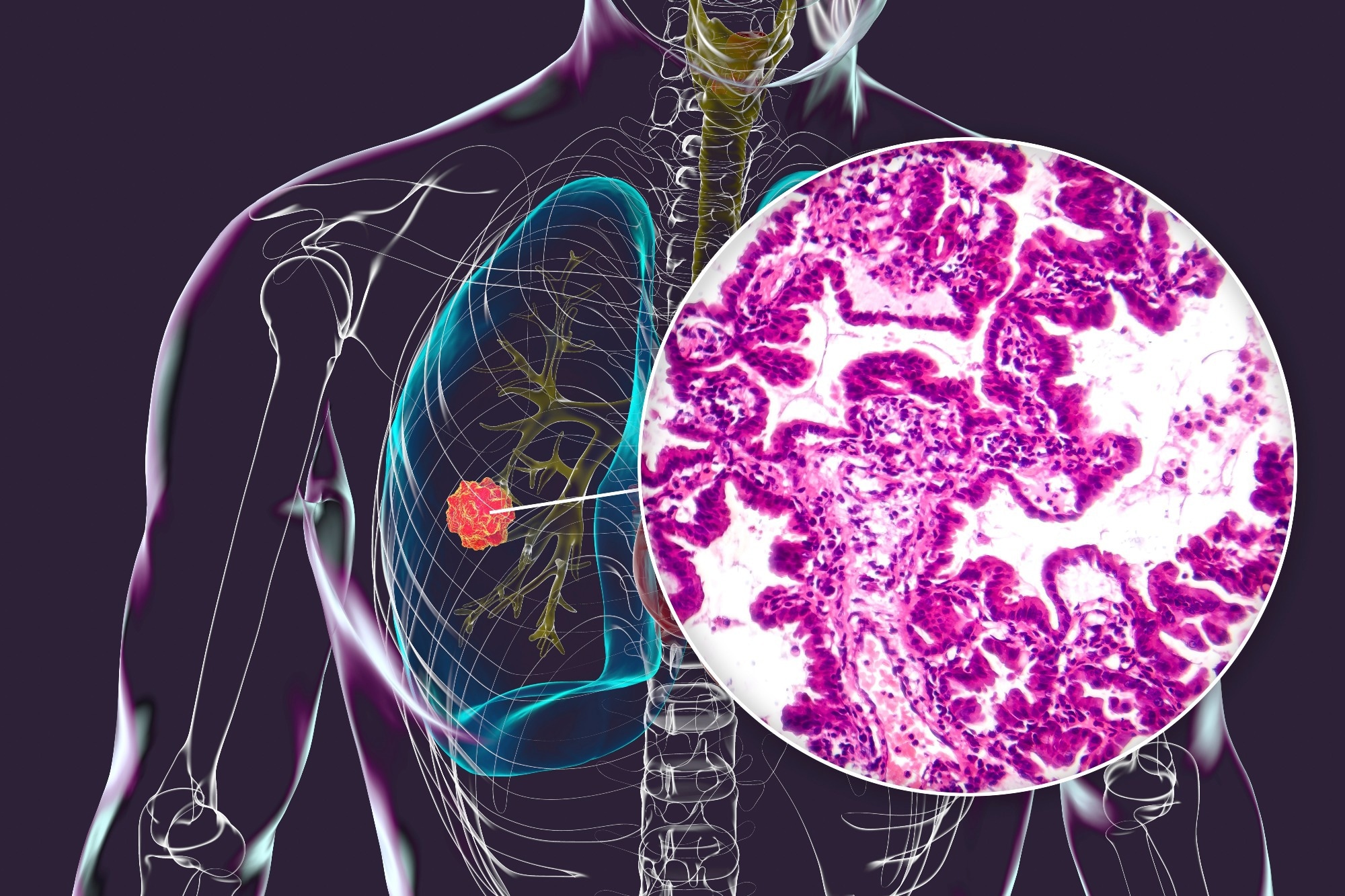 Study: Real-world deployment of a fine-tuned pathology foundation model for lung cancer biomarker detection. Image credit: Kateryna Kon/Shutterstock.com
Study: Real-world deployment of a fine-tuned pathology foundation model for lung cancer biomarker detection. Image credit: Kateryna Kon/Shutterstock.com
A recent Nature Medicine study compiled a large international clinical dataset of digital lung adenocarcinoma (LUAD) slides to facilitate the development of a computational epidermal growth factor receptor (EGFR) biomarker.
Testing for EGFR mutations in lung adenocarcinoma
LUAD is the most prevalent form of lung cancer, with EGFR being the most common somatic mutation in kinase genes. Accurate EGFR testing is crucial to ensure patients receive the correct first-line therapy. EGFR testing is done for patients with advanced-stage LUAD; otherwise, molecular testing in lung cancer is the standard line of investigation. EGFR testing is significantly below the level determined by clearly published guidelines. There could be many reasons, including technical hurdles in obtaining and processing samples for testing and insufficient material from diagnostic biopsies.
Computational methods to detect EGFR mutations can significantly improve the clinical workflow for lung cancer diagnostic biopsies. Only the digitized pathology slides from the diagnostic Hematoxylin and Eosin (H&E) biopsy would be used as a substrate, enabling the result to be reported with no physical processing and little cost. The immediate production of results should also allow for informing all other downstream decisions.
About the study
This study developed the EAGLE (EGFR AI Genomic Lung Evaluation) and showcased its clinical usefulness as an H&E-based computational biomarker. The goal was to enhance the standard molecular workflow by using the diagnostic biopsies of LUAD patients to predict the EGFR mutational status. Unlike the traditional workflow, AI-assisted screening often precludes rapid testing. This was done while maintaining overall high screening performance. Next-generation sequencing (NGS)- based testing was still required for samples that were screened positive.
A large international clinical dataset of digital lung adenocarcinoma (LUAD) slides was compiled to train the algorithm in line with the broad biological and technical variability expected from real clinical deployment. A total of 5,174 slides from the Memorial Sloan Kettering Cancer Center (MSKCC) were used to fine-tune a state-of-the-art pathology foundation model. Model validation was done using 1,742 internal slides from MSKCC and on external test cohorts to ensure robustness.
These included institutions in the United States and Europe and spanned multiple slide scanners, demonstrating the model's generalizability across institutions and multiple scanners. A silent trial was conducted by deploying EAGLE in real time to simulate its performance in a real-world setting.
Study findings
EAGLE performed at the expected level on novel cases and was deemed suitable for clinical implementation. The results of the EGFR rapid test were compared with the results of the Idylla test. Idylla showed a positive predictive value (PPV) of 0.988, sensitivity of 0.918, specificity of 0.993, and a negative predictive value (NPV) of 0.954 in the period analyzed. The model achieved an area under the curve value (AUC) of 0.847. The performance was less accurate in metastatic specimens (AUC 0.75) compared to primary samples (AUC 0.90).
Using tissue amount as a proxy for tumor amount, the surface area was calculated based on the tiles used for model inference. A general trend was noted, whereby the model performance was enhanced as the area of the analyzed tissue increased. Further tests revealed that the model was able to detect all of the clinically relevant EGFR mutations, thereby highlighting the robustness of EAGLE across variants. The model's performance on external cohorts was also in line with the internal validation and showed an AUC of 0.870.
A silent trial was run at MSKCC to test real-world applicability. As in the previous case, the model performance was lower in metastatic specimens (AUC 0.760), compared to primary samples (AUC 0.896). Lymph nodes (AUC 0.74) and bones (AUC 0.71) performed particularly poorly. The overall AUC was comparable to previous results at 0.853. These results further supported the deployment of EAGLE for primary samples. The artificial intelligence (AI)-assisted workflow could lead to a lower number of samples being rapidly tested, based on the output of EAGLE.
Three threshold strategies were explored in the trial to determine how many rapid tests could be spared while maintaining performance comparable to traditional workflows. Depending on the chosen threshold, the AI-assisted workflow reduced rapid tests by 18% to 43% while preserving high NPV and PPV values.
The turnaround time for EAGLE was also a key advantage, delivering results in a median of just 44 minutes, significantly faster than the minimum 48 hours needed for rapid testing and several weeks for NGS.
The real-world setting silent trial was important as it helped researchers understand how the newly devised protocol performed, including possible sources of false negative and false positive results. By examining attention heatmaps overlaid on tissue slides, the team identified that false positives often involved biologically related mutations like ERBB2 insertions or MET exon 14 skipping events. False negatives tended to occur in samples with minimal tumor architecture, such as cytology specimens or blood-heavy biopsies.
It was hypothesized that the error rate could be lowered significantly if pathologists manually interpreted the results. The EAGLE is not intended to replace NGS sequencing but is only a screening test. EAGLE is meant to identify likely positive cases and efficiently rule out EGFR mutations. Because EAGLE does not distinguish between EGFR subtypes that require different targeted therapies, NGS confirmation is still necessary before treatment selection.
Conclusions
This study presented a validated computational pathology model for detecting EGFR mutation in LUAD. The model can reduce tissue consumption, improve diagnostic efficiency, and accelerate AI adoption in clinical practice. EAGLE achieved its performance by fine-tuning a vision transformer-based foundation model, highlighting a shift toward more generalizable AI tools in pathology. Future research should consider additional biomarkers and study them in a prospective clinical trial.
Download your PDF copy now!
Journal reference:
- Campanella, G., Kumar, N., Nanda, S. et al (2025). Real-world deployment of a fine-tuned pathology foundation model for lung cancer biomarker detection. Nature Medicine. Doi: https://doi.org/10.1038/s41591-025-03780-x. https://www.nature.com/articles/s41591-025-03780-x