Food allergies affect approximately 8% of school children in the United States and the United Kingdom. The highest prevalence of food allergies is in Australia affecting approximately 10% of young children. It is lower in the developing world.

What are the main foods that people are allergic to?
The main food allergies that affect young children include:
- cow’s milk
- egg white
- peanut
- fish
- wheat
The main allergies affecting adults are:
There are geographical differences with peanut allergy being far more prevalent in some countries than in others.
Mustard allergy is an important cause of food allergies in children in France; whereas wheat and buckwheat allergies are important causes of food allergies in children in Japan.
How much is currently known about how food allergies, such as peanut allergy, arise?
There are various theories that have been put forward to explain the rise in food allergies, including the Hygiene Hypothesis, the vitamin D Hypothesis, and the Dual Allergen Exposure Hypothesis.
The Hygiene Hypothesis in its most modern form suggested there is a dysbiosis or imbalance in our gastrointestinal microflora and that in the absence of high microbial diversity, immune dysregulation occurs leading to allergies.
The vitamin D Hypothesis posits that insufficient sunlight exposure leads to low vitamin D levels and a dysregulation of the immune system with deficiencies in the function of regulatory T cells.
There is increasing evidence now for the Dual Allergen Exposure Hypothesis. This posits that in the absence of early oral tolerance through consumption of peanuts and other food allergens, exposure to food allergens through a broken down skin barrier (e.g. in children with eczema) in the first year of life leads to allergic sensitisation.

More than 80% of children with peanut and tree nut and egg allergies have a preceding history of eczema and it is thought that the defect in the skin barrier in these children allows penetration of food allergens in the environment. In contrast, early oral exposure of foods, at least to peanut, leads to oral tolerance.
It is therefore likely that the increase in peanut allergy has been caused by a combination of factors: an increase prevalence of eczema and increasing severity of eczema over the past few decades in infancy, and increasing vigilance on exclusion from dietary allergens from the diet of young infants during the first year of life.
What research is being conducted into preventing and treating food allergies?
The LEAP and EAT studies are being continued with follow up of the same cohort of children to see whether effects of early consumption of foods on food allergy prevention are sustained into later childhood. While there is conclusive evidence that oral tolerance induction to peanut protects against peanut allergy, this remains to be established for other foods.
The next few years will see the development of new prevention studies focusing on egg and milk through oral tolerance induction. A variety of other approaches are also now open to consideration especially relating to preservation of skin barrier function.
What is immunotherapy?
Immunotherapy is a form of allergen specific desensitization. It has been practised for many decades to treat allergic rhinoconjunctivitis especially in relation to hay fever. The treatment involves administering increasing amounts of allergen over several years to cause desensitisation and symptom reduction. This has been shown especially in respiratory allergies to have long term benefit and affect the natural history of allergic disease.
In recent years, oral immunotherapy to foods, especially peanut, egg, and milk have shown promising results with significant increases in the threshold of food tolerated by the allergic individual. This strong protective effect is however accompanied by allergic side effects and does not appear to result in long term disease remission for the majority of children who require ongoing consumption of the food allergen in order to remain desensitised.
The most recent form of immunotherapy to peanut is currently under intensive investigation in phase 3 clinical trials and this involves epicutaneous immunotherapy (via a peanut protein patch) to reduce reactivity to peanut.
Phase 1 and 2 clinical trials suggest that this approach may be efficacious in children with peanut allergy. If this therapy is successful in the phase 3 clinical studies, an important advantage of this treatment would be that it is associated with very mild local side effects compared to oral immunotherapy, while achieving protection against accidental oral exposure.
How does immunotherapy compare to other potential treatment and prevention options for food allergies?
Currently apart from allergen specific immunotherapy, there are no good options to treat and prevent food allergies. There is the potential for new biologics but the best current options we have are to focus on safe and effective ways of delivering allergen specific immunotherapy.
What are the main hurdles that need to be overcome to advance our understanding of food allergies and how they can be treated or prevented?
Understanding the role of the skin barrier in the development of food allergy, prevention of food allergy, and treatment of food allergy will be fundamental to understanding the pathogenesis of food allergies, and will lead to enhanced therapies.
We will also need to learn how to make the effects of immunotherapy to food allergen long lasting and whether this can be achieved simply through a long period of immunotherapy to the food or will require the addition of another treatment modality.
What do you think the future holds for food allergies?
We have reached an important crossroads in our understanding of food allergies and how to prevent food allergies. The last decade has also seen a significant body of research pointing to the role of immunotherapy in food allergy. It is an exciting time for the field and I am very optimistic about the prevention and treatment of food allergies moving forward and reducing the societal burden of food allergy.
Where can readers find more information?
About Professor Gideon Lack
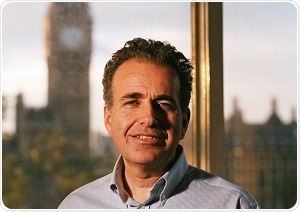 MD, MA, MBBCH, FRCP, CH
MD, MA, MBBCH, FRCP, CH
Gideon Lack, MBBCH (Oxon) MA (Oxon), FRCPCH, Professor of Paediatric Allergy, King’s College London, Head of the Clinical Academic Paediatric Allergy Service, Guy’s & St. Thomas’ NHS Foundation Trust
Clinical Academic Paediatric Allergy Service at Guy’s & St. Thomas’ NHS Foundation Trust. He read medicine at Oxford University before training as a Paediatrician in New York, and specialised in Paediatric Allergy in Denver, Colorado.
His research focuses on peanut allergy and strategies to prevent peanut and food allergies through oral tolerance induction. The LEAP study showed that early consumption of peanuts in atopic infants reduces the development of peanut allergy by >80%. His research shows that allergic sensitisation to food may occur through an impaired skin barrier and is studying the mechanisms of cutaneous sensitisation and oral tolerance.