Errors with the metabolism of cells can cause a multitude of different cancers. The metabolic mechanisms in cancerous cells can be forcibly hijacked to further support the cancerous phenotype of these cells.
Fortunately, the metabolism of cancerous cells can be manipulated to provide therapeutic treatment for these cancers.
Cancer risk and metabolism
The idea that cancer is caused by dysfunctional proliferation is widely accepted and supported by the literature. Furthermore, recent discoveries provided from research has shown that metabolic disorders also contribute to the development of various cancers.
Tumor cancer cells attacking and growing on human cell 3d rendering. - Illustration Credit: Illustration Forest / Shutterstock
Otto Warburg showed that the metabolism of tumor cells varied greatly compared to non-cancerous cells. His research discovered a significant difference in energy consumption between normal and tumorous cells. For normal cells, most pyruvate is oxidized via oxidative phosphorylation after it enters the tricarboxylic acid cycle. On the other hand, tumor cells convert most of their pyruvate into lactic acid which produces energy anaerobically. This is called aerobic glycolysis or the Warburg effect.
Cancer cells evade glycolytic regulatory mechanisms in many different ways. Additionally, cancer cells are able to evade the attention of control mechanisms that limit the rate of glycolysis. This is demonstrated when phosphofructokinase (PFK) becomes less sensitive to ATP inhibition in cancerous cells, which results in no decrease of glucose concentrations in cancerous cells leading to an overly metabolically active cell. Cancer cells can also induce an increased rate of glycolysis by increasing the levels of fructose-2,6-biphosphate.
There are numerous other changes to the metabolism in cancerous cells. Some of which include:
- Increased citrate generation
- Increased intracellular and extracellular lactate generation
- Increased intracellular glucose and glutamine generation
Evidence has shown that elevated glucose consumption and increased lactate secretion in tumor cells contributes to the growth of a tumor. This is exemplified by the increased risk of developing certain cancers (e.g. pancreatic, gastrointestinal tract, liver, colon, and breast cancer) for individuals with elevated blood glucose due to type 2 diabetes mellitus.
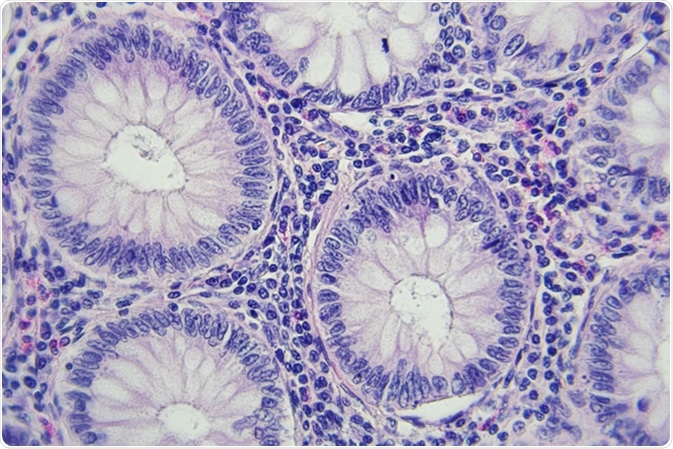
Colon cancer microscopic photography, magnification x400. Image Credit: Lukasz Pawel Szczepanski / Shutterstock
Using quantitative tandem mass spectrometry (MS/MS) to analyze the blood and tissues of breast cancer patients, researchers have been able to demonstrate that a specific metabolic phenotype can be used to identify those at risk for breast cancer. These metabolic differences were accordant with the congenital errors of metabolism that are seen in certain types of breast cancers. The findings of this study could be used to identify breast cancer type with an accuracy of 95%. These findings show that quantitative MS/MS can effectively be used as a breast cancer early detection method.
Inhibiting the expression of various glucose transporters (e.g. glucose transporter 2 [GLUT2], lactate dehydrogenase [LDH], or PDK) decreases tumorgenicity when performed with xenograft models. Also, knocking down the β-catalytic subunit of mitochondria H+-ATP synthase increases the glycolytic rate resulting in a more aggressive tumor-forming phenotype. These properties clearly portray the importance of the glycolytic phenotype in tumor development.
Using tumor metabolism as a therapeutic target for cancer treatments
Some current anticancer therapies involve specifically targeting an activated oncogene with the aim to achieve remission of cancer. Unfortunately, the cancer returns for many patients which shows that these types of treatments aren't completely effective and that cancers are very persistent. Metabolic-based cancer therapies may be more effective at treating cancer than gene-based therapies as shifts to metabolism are seen in more tumors than changes to genes, also resistance to metabolic-based therapies are less common than resistance gene-based ones.
Multiple methods aimed at reducing the glycolytic flux of tumor cells are being discussed as cancer therapies. These include:
- Low-carbohydrate diets to reduce extracellular glucose levels
- Lonidamine to inhibit the glucose to hexose conversion
- Using PKM2 activators/inhibitors to regulate pyruvate levels
Targeting glutaminolysis is another method by which themetabolic activity of cancerous cells may be reduced. This suppression may be achieved by inhibiting glutamine transporters (I.e using the retinoblastoma protein to downregulate the Na+-coupled glutamine transporter [SLC1A5]). As glutaminolysis starts with the conversion of glutamine to glutamate by glutaminase (GLS), regulating the activity of GLS can be used to treat certain cancers. This can be achieved by targeting c-Myc which regulates the transcription of GLS. NF-κB and the MAPK (ERK) signaling also regulated the activity of GLS, therefore can be used as therapeutic targets for cancer.
Many studies indicate that inhibiting the growth of tumors can be achieved by impeding glycolysis to force pyruvate towards oxidative pathways and reduce lactate generation.
The drawbacks of using metabolic-based therapies is that they often cause non-specific toxicity to normal healthy tissues and cells. These anticancer therapies may target cells of the immune system which will reduce the immune response towards the tumor. Toxicity is also exhibited in neuronal cells as reducing glucose levels can cause neuropathies as neurons are very energy intensive, requiring large amounts of glucose.
Further Reading
Last Updated: Jul 1, 2019