The current pandemic of COVID-19 is caused by the severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2), a betacoronavirus similar to that which caused the SARS-CoV and MERS-CoV earlier. Scientists are pursuing therapeutic drugs and vaccines to counter the relentless spread of the virus, but so far, none has been established to be effective. However, several are in clinical trials in various parts of the world.
The SARS-CoV-2 is an RNA virus with a genome that concerns 4 structural proteins: the envelope (E) protein, the spike (S) protein, the membrane (M) protein, and the nucleocapsid (N) protein. There are also 16 non-structural proteins and several accessory proteins. The S protein is the major protective antigen against which the host produces neutralizing antibodies, and has been the primary target of most vaccine developers.
Prior Vaccine Attempts
For instance, an inactivated viral vaccine was found to produce neutralizing antibodies against multiple strains of the virus, protecting macaques against this infection. A chimpanzee adeno-vectored (ChAD) vaccine containing the full S gene of the virus produced both cellular and humoral reactions in macaques. Still, it could not completely mitigate the clinical features, though it did produce a significant decline in the severity of pneumonia.
A similar failure was seen with the ChADOx1 nCoV-19 vaccine, which allowed the current virus to replicate in the nose, with its sinister implications of vaccinated people still spreading the virus through sneezes.
Inherent Advantages of AOaV-1
However, the avian orthoavulavirus 1 (AOaV-1) presents several advantages as a vaccine vector. For one, it is a cytoplasmic virus, which means the viral genome will not be incorporated into the host genome – a hugely safer means of vaccination. Secondly, the lack of natural recombination allows for genetically stable expression of the transgenes. It has a restricted host range, and induces a strong interferon expression in mammalian cells, thus preventing its replication.
Thirdly, the AOaV-1 can infect multiple animal species, which means that it can be grown in multiple cell lines. With all these features, harmless strains of AOaV-1 have been used as live attenuated vaccines against many viral infections like influenza, Nipah disease, Ebola, and avian flu.
The natural host of AOaV-1 is avian, and the vector has different antigens from the pathogens that commonly infect humans, which means there is no pre-existing human immunity. This makes it suitable for human transfection.
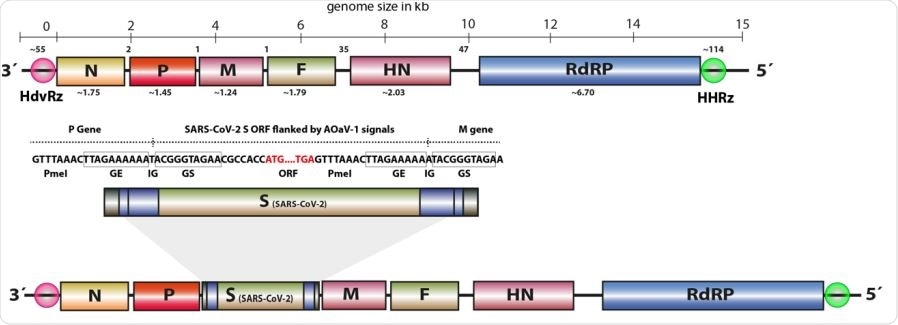
The full-length ORF for S gene of SARS-CoV-2 was over596 hanged with required transcriptional signals (GE, GS, IG) and inserted in between P 597 and M genes. The rough gene size is mentioned below each gene, the division of the 598 genome across the length and number of nucleotides in intergenic region is displayed 599 at the top of the schema of the AOaV-1 genome.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Recombinant AOaV-1 Strain
For the current study, the researchers designed an AOaV-1 vector from an avirulent strain of the virus, containing the complete antigenomic sequence of the AOaV-1 derived from wild birds with asymptomatic infection. Within this viral vector, the whole Spike protein gene was expressed at an optimized gene junction. In vitro studies were carried out to fully characterize this vaccine, its sensitivity to antibodies, its replication and stability within embryonated chicken eggs.
The next step was to test the vaccine for safety and immunogenicity using an animal model. The construct was termed rAOaV-1-SARS-CoV-2, and the wildtype strain without the S gene insert was called AoaV-1-wt. Both were propagated in embryonated chicken eggs at 8 days of age. These eggs were then screened to identify the successfully propagated viruses.
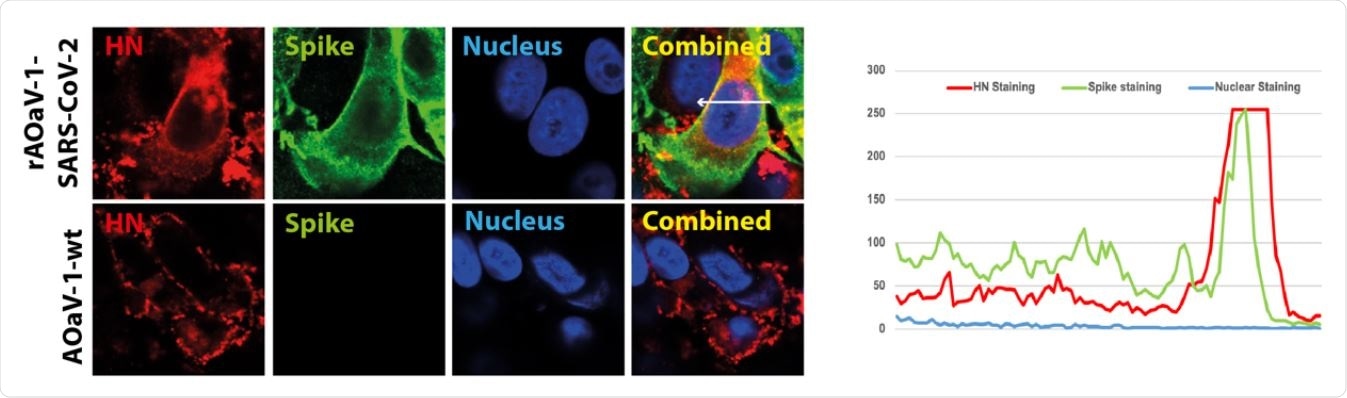
Vero cells were infected with the 600 AOaV-1-wt or rAOaV-1-SARS-CoV-2 and sainted for the expression of the HN (red) 601 or S (green) proteins. The co-expression of both surface proteins is coloured yellow in 602 combined images and Quantitative co-expression profile is marked with arrow and 603 shown in the line chart.
The Results of the Recombinant Vaccine Propagation
The S protein and HN protein was identified in the cells infected with the rAOaV-1-SARS-CoV-2 strain, which showed that the recombinant vaccine could express both the transgenic S protein and its own growth proteins.
The replication of AOaV-1 can occur only after cleavage of its F protein by cellular proteases. To find out if exogenous trypsin or similar proteases were necessary for the infectivity of this virus, the researchers used the recombinant strain and the wildtype strain to infect cell cultures in the absence of trypsin.
The recombinant virus replicated and spread to neighboring uninfected cells within 12 hours, with up to 90% of cells being infected within 2 days of infection. Most of the cells expressed both the HN and S protein. The slow spread of the infection was confirmed by cumulative fluorescence dynamics, which identified either the HN or the S protein and thus displayed the presence of both on the surface of the infected cells.
Thus, the recombinant vaccine, as well as the wildtype virus actively replicated and spread to a comparable extent without exogenous trypsin, expressing both native and foreign genes in the host cells.
The incorporation of the S protein into the recombinant virus led to its neutralization by anti-SARS-CoV-2 antiserum and more strongly by anti-AOaV-1 antiserum, at about 40% and 90% respectively.
Finally, the study showed that the S protein was stably expressed in the recombinant vaccine even after multiple passages in the chicken embryonated eggs, but the growth characteristics in vitro were maintained to a large extent.
Suitability of the Viral Vector for Vaccine Development
Overall, therefore, the vaccine candidate is highly attenuated in primate species am is pretested. It can express the antigenic S protein, is able to propagate and replicate stably over the course of several successive passages in embryonated chicken eggs, and still maintain normal growth characteristics in vitro. This gives it “the potential for accelerated vaccine development against CoVID-19 for clinical studies.”.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources