The coronavirus disease (COVID-19) pandemic is actively spreading across nations, with millions of people affected. In the United States alone, more than 7.45 million people have been infected, and more than 210,000 have died.
The country has seen that the pandemic has disproportionately affected racial and ethnic minority communities, prompting the research team from Harvard Medical School to determine the individual and census tract-level sociodemographic and economic factors, which have been tied to COVID-19 infection.
The study, published on the open-source preprint server medRxiv*, aimed to determine the role several individual and social factors could increase the risk of COVID-19 infection.
Many health experts believe that factors may contribute to the risk of infection and potential adverse outcomes, including language barriers, lower health literacy, household overcrowding, reliance on public transport, and limited financial access to healthcare, among others.
The study
To arrive at the study findings, the research team analyzed findings from more than 57,000 people. They measured individual factors, such as age, sex, and race, while also considering census tract- level factors, like population density, how many people are living in the household, and education status, and how these factors could increase the risk of contracting the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19.
The team obtained demographics, laboratory values, diagnoses, hospitalizations, and deaths from the electronic medical record (EMR) of Mass General Brigham, an extensive healthcare system in Eastern Massachusetts. The sociodemographic data, on the other hand, was obtained from the 2014-2018 American Community Survey (ACS).
The participants included in the study were those who tested positive for COVID-19 via the viral polymerase chain reaction (PCR) test in the MGB between February 1 and June 21, which was a window of beginning about two months before and ending three months after the peak of the cases in the state.
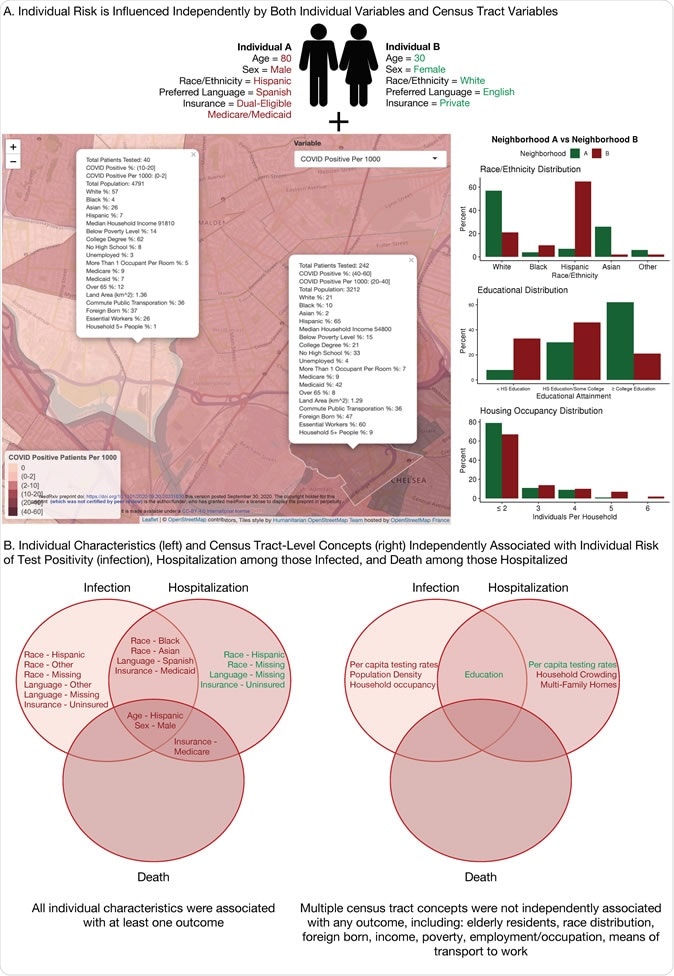
(A) Conceptual model of an individual’s aggregate risk of disease, arising from the interaction between individual and census tract-level risk factors, with red indicating a positive association with adverse outcomes (increased risk) and green indicating a negative association (decreased risk), and (B) summary of individual characteristics (left) and census tract-level concepts (right) which were independently associated with infection with SARS-CoV-2, hospitalization among those infected, and death among those hospitalized within our study sample, with red indicating a positive association with adverse outcomes (increased risk) and green indicating a negative association (decreased risk). HS = high school.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
The study findings
The study outcomes included the risk of infection with the coronavirus, hospitalization tied to COVID-19 among those who tested positive, and death among those hospitalized.
The researchers found that being older, male, non-White race, non-English, and those with non-private insurance, were at a higher risk of COVID-19 infection. Further, in the census tract-level, the team revealed that those who are living in areas with an increased population density, more people living in the same house, and lower educational level were also tied to a higher risk of contracting SARS-CoV-2.
In terms of hospitalization, the team also found that people in more multi-family homes, extreme household crowing, and lower education were tied to an increased risk of hospitalization. Also, only individual level-factors, such as old age, being male, and having Medicare insurance, have been associated with increased risk of death among those who were hospitalized.
“This study of the first wave of the SARS-CoV-2 pandemic in a major U.S. city presents the cascade of outcomes following SARS-CoV-2 infection within a large, multi-ethnic cohort,” the research team concluded in the study.
“SARS-CoV-2 infection and hospitalization rates, but not death rates among those hospitalized, are related to census tract-level socioeconomic characteristics including lower educational attainment and higher household crowding and occupancy, but not neighborhood measures of race, independent of individual factors,” they added.
COVID-19 high-risk individuals
Nine months into the pandemic, the list of those who are at a higher risk of COVID-19 infection, and those who may develop severe symptoms have expanded. Early in the pandemic, older adults and those with underlying medical conditions were tagged as high-risk individuals. Many studies showed that males are also at a higher risk of COVID-19, and in the United States, minorities are more affected by the pandemic since they are also at a higher risk of developing severe COVID-19.
Globally, the coronavirus pandemic is far from over, with more than 35.34 million infections since December 2019, when the coronavirus first emerged in Wuhan City in China.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Source:
Journal reference: