Researchers at Yale University and other major institutions found that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral loads in saliva are higher for patients with associated risk factors and underlying conditions that lead to severe coronavirus disease 2019 (COVID-19) and death. Thus, saliva viral loads could be used to predict disease severity.
The symptoms and severity of COVID-19, the disease caused by the SARS-CoV-2, differ widely among patients. Some patients are asymptomatic, while in others, the condition becomes severe, requiring medical intervention and can also lead to death.
Severe manifestations of the disease have been mainly seen in older men who also have other diseases. In these cases, patients show a strong inflammatory response, and production of cytokines and chemokines. However, it is still not clear which factors affect disease severity and can explain the different cellular, immunological, and demographic parameters observed.
Testing for the virus has revealed that samples obtained from the nose, throat, saliva, urine, and stool have different viral loads. Generally, higher nose and throat viral loads have been associated with greater disease severity and with inflammatory factors.
Testing viral loads in saliva
Saliva can be a useful alternative for COVID-19 testing. In a new study published on the medRxiv* preprint server, researchers report the relationship between saliva viral loads and COVID-19 risk factors and disease symptoms.
The authors tested the viral loads, cytokines, chemokines, and antibodies in saliva, nose, and throat samples from 154 patients admitted to the Yale-New Haven hospital between March and June 2020. Of these patients, 62 had severe disease, 84 had moderate symptoms, and 23 patients died. Apart from these patients, the study also included other patients who were COVID-19 positive but did not require hospitalization.
The authors then analyzed the viral loads obtained to see if there is a link between the viral loads and risk factors like sex, age, and cardiovascular or other immune-suppressive conditions.
They found the saliva viral loads to be significantly higher in patients with chronic respiratory conditions, cardiovascular conditions, kidney disease, and diseases that compromise the immune system. Patients with four or more risk factors had much higher saliva viral loads than patients with fewer risk factors, as did male patients. However, there was no relation between nose and throat viral loads and the risk factors. Saliva viral loads were also higher in patients with worse clinical outcomes.
Data analysis revealed that the saliva viral loads combined with days after symptom onset could predict disease severity and death in the hospitalized patients, while nose and throat swabs could not.
The authors also studied the relationship between viral loads and immunological factors such as cytokines, platelets, and antibodies. Saliva, nose, and throat viral loads all showed a strong correlation with interferons, cytokines, and other chemokines, with the saliva viral loads showing a stronger relation than nose and throat viral loads. Saliva viral loads also showed a strong correlation with IL-8 and IFNl, factors that have been associated with disease severity and death. Patients with higher saliva viral loads showed a lower number of lymphocytes and T cells.
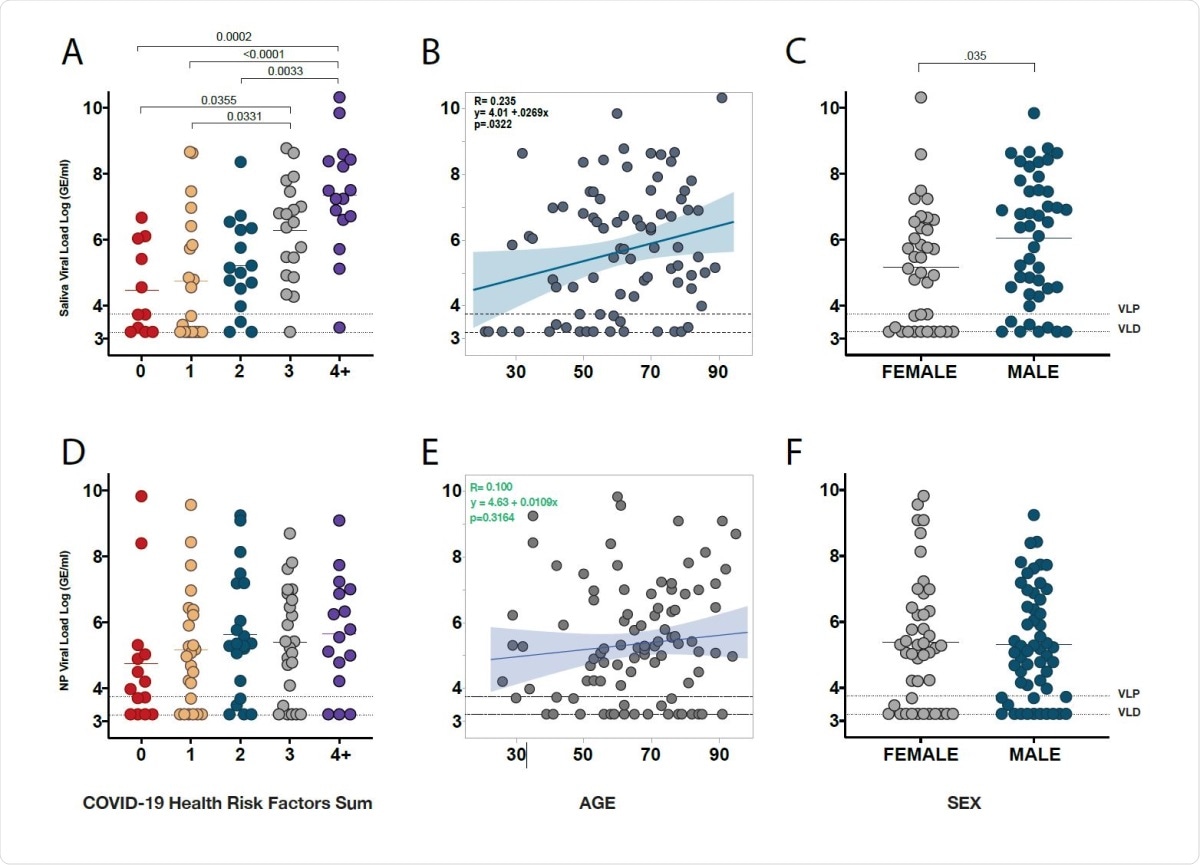
Saliva viral load, but not NP Viral Load, increases with COVID-19 health risk factors, age, and is higher in males.
There was a negative correlation between saliva viral loads and antibodies. Patients with low or moderate saliva viral loads had higher IgG antibodies to the virus spike protein and receptor-binding domain (RBD). Furthermore, patients with higher saliva viral loads started producing antibodies slower than patients with low saliva viral loads.
Monitoring virus in saliva could help better manage COVID-19
Thus, patients having higher saliva viral loads initially needed higher antibody concentrations to overcome the infection. Although anti-RBD IgG brought down saliva viral loads, a broader anti-S1 IgG was needed to overcome the infection. Initially, high saliva viral loads and higher loads for longer periods could indicate higher COVID-19 disease severity.
The results suggest there is a distinct virus replication process in the saliva compared to the nose and throat. Collection of the virus in the saliva may also indicate viral replication in vital organs. For example, it may indicate virus infection and replication in the lower respiratory tract that reaches the mouth through mucus clearance processes and mixes with the saliva.
These findings may serve as a window to apply and monitor interventions dedicated to reducing viral load early before severe depletion of effector cell populations in days 10-20 from symptom onset,” write the authors.
The mixed results of some drugs and antibodies to reduce viral loads could be related to their inability to lower viral loads in the early stages of the disease.
As patients with higher viral loads need higher antibody levels to lower virus levels, this will be important to consider when administering convalescent plasma or antibody therapies. Providing therapies early to reduce virus loads, within 10–20 days of symptom onset, will allow a better immune response and recovery.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources