Researchers based in Beijing and Shenzhen, China, report that they have identified mutations in the spike protein of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that may allow variant strains to avoid neutralization by monoclonal antibodies and convalescent blood plasma.
A pre-print version of the research paper is available to read in full on the bioRxiv*server.
Virus neutralization in humans
Zhang and colleagues assembled a panel of 28 SARS-CoV-2 pseudoviruses containing single or combined mutations in the spike protein that can be found in the variants UK501Y.V1, SA501Y.V2 and BR501Y.V3 variants, first identified in the United Kingdom, South Africa, and Brazil, respectively. The pseudoviruses were then tested against a panel of monoclonal antibodies (mAb) and convalescent patient blood plasma, acquired during the first wave of the coronavirus disease 2019 (COVID-19) outbreak.
The team found that the South African variant, which contains a triple K417N-E484K-N501Y mutation, was able to significantly resist mAbs and convalescent plasma.
To replicate, the SARS-CoV-2 virus structure binds to an angiotensin-converting enzyme 2 (ACE2) on a cell membrane. This enzyme can predominantly be found on heart, lung, and kidney cells and has a role in lowering blood pressure.
The researchers found that the single K417N mutation provided substantial mAb resistance, however it reduced the ability of the virus to bind to ACE2 by 6.4-fold. The E484K mutation also provides neutralization resistance by forming salt-bridges or hydrogen bonds, rendering antibodies ineffective. The N501Y mutation sharply increases binding affinity, and thus as such when the three mutations are combined (K417N-E484K-N501Y), the new mutant strain is both more transmissible and more resistant to neutralization from a wide range of antibodies.
The same mutant strains were tested in convalescent blood plasma from SARS-CoV-2 infected individuals. Twenty-three samples were acquired from hospitalized patients between January and February of 2020. A lack of detectable neutralization activity occurred in 11 of the plasma samples for the SA501Y.V2 pseudovirus, 4 for the BR501Y.V3, and none of the UK501Y.V1. The remaining plasma was observed to have varying degrees of neutralization.
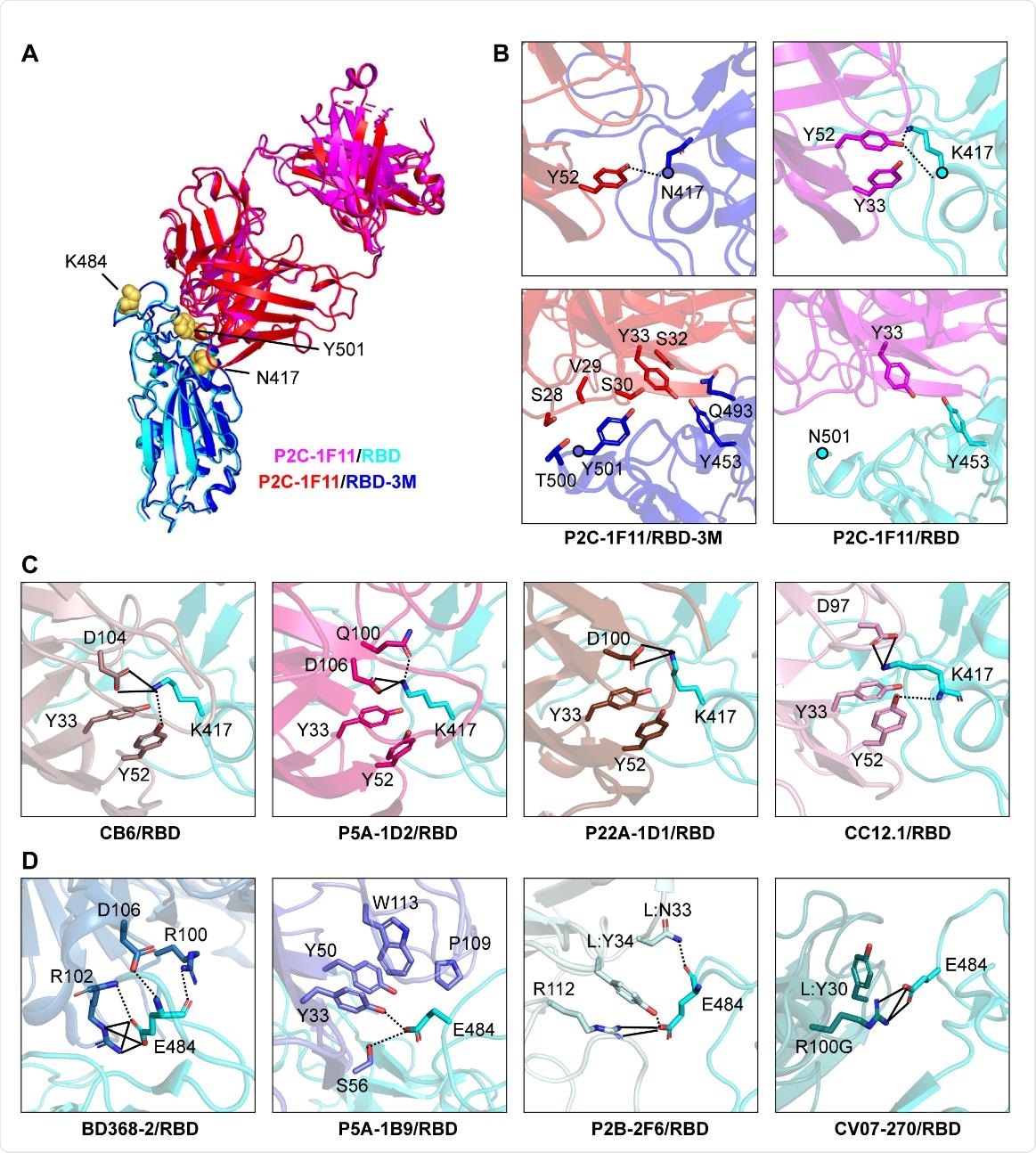
Structural basis for mAb neutralization and escape. (A) P2C-1F11/RBD224 3M crystal structure superposed onto P2C-1F11/RBD crystal structure (PDB: 7CDI). P2C-1F11 is colored with magenta and RBD is colored with cyan in the P2C-1F11/RBD complex. The P2C-1F11 and RBD-3M are colored with red and blue respectively in the P2C-1F11/RBD-3M complex. The three RBD-3M mutated residues (N417, K484, and Y501) are shown as yellow-colored spheres. (B) Interactions with P2C-1F11 around RBD-3M N417 and Y501 (left panel) and wildtype RBD K417 and N501 (right panel). (C) Interactions between K417 and representative Class I IGHV3-53/3-66 antibodies CB6, P5A-1D2, P22A-1D1 and CC12.1. (D) Interactions between E484 and Class II antibodies BD368-2, P5A-1B9, P2B-2F6 and CV07-270. For panel (C) and (D), antibodies are shown with different colors; hydrogen bond and salt bridge are represented by dashed and black lines, respectively. CB6/RBD (PDB: 7C01), P5A235 1D2/RBD (PDB: 7CHO), P22A-1D1/RBD (PDB: 7CHS), CC12.1/RBD (PDB: 6XC2), BD368-2/RBD (PDB: 7CHC), P5A-1B9 (PDB: 7CZX), P2B-2F6 (PDB: 7BWJ), CV07-270 (PDB:6XKP).

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Onto animals
The researchers went on to further test the range of cross-species transmission of the variant pseudoviruses. They were able to identify nine host species to which the 28 pseudoviruses were able to bind to ACE2. They found that the E484K mutation allowed for enhanced entry into mouse- and mink-ACE2.
This ability for SARS-CoV-2 to transmit itself across species raises concerns that local wildlife epidemics could break out or simply that humans that interact with animals in a native setting that either individual could cross-infect the other. As such, the authors of the study insist that monitoring and thorough surveillance of relevant animal species is necessary in order to prevent future outbreaks.
Keeping mutants under control
Zhang and colleagues specifically make aware the fact that antigenic shifts are occurring in emergent SARS-CoV-2 variants and that vaccines aimed at neutralizing the original Wuhan-Hu-1 wildtype strain are ineffective against rising mutations. As such, research should be directed to finding a vaccine or antibody treatment that works widely across the whole spectrum of emergent COVID variants.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.