Researchers at Rutgers School of Dental Medicine have found evidence that two types of mouthwash disrupt the COVID-19 virus under laboratory conditions, preventing it from replicating in a human cell.
The study, published in the journal Pathogens, found that Listerine and the prescription mouthwash Chlorhexidine disrupted the virus within seconds after being diluted to concentrations that would mimic actual use. Further studies are needed to test real-life efficacy in humans.
The study was conducted in a lab using concentrations of the mouthwash and the time it would take to contact tissues to replicate conditions found in the mouth, said Daniel H. Fine, the paper's senior author and chair of the school's Department of Oral Biology.
The study found two other mouthwashes showed promise in potentially providing some protection in preventing viral transmission: Betadine, which contains povidone iodine, and Peroxal, which contains hydrogen peroxide. However, only Listerine and Chlorhexidine disrupted the virus with little impact on skin cells inside the mouth that provide a protective barrier against the virus.
Both Povidone iodine and Peroxal caused significant skin cell death in our studies, while both Listerine and Chlorhexidine had minimal skin cell killing at concentrations that simulated what would be found in daily use."
Daniel H. Fine, Paper's Senior Author
The team studied the efficacy of mouthwash potential for preventing viral transmission to better understand how dental providers can be protected from aerosols exhaled by patients. "As dentists, we're right there in a patient's face. We wanted to know if there's something that might lower the viral load,'' said coauthor Eileen Hoskin, an assistant professor at Rutgers School of Dental Medicine.
Fine cautions the public against relying on mouthwash as a way to slow the spread until it is proven in clinical trials on humans.
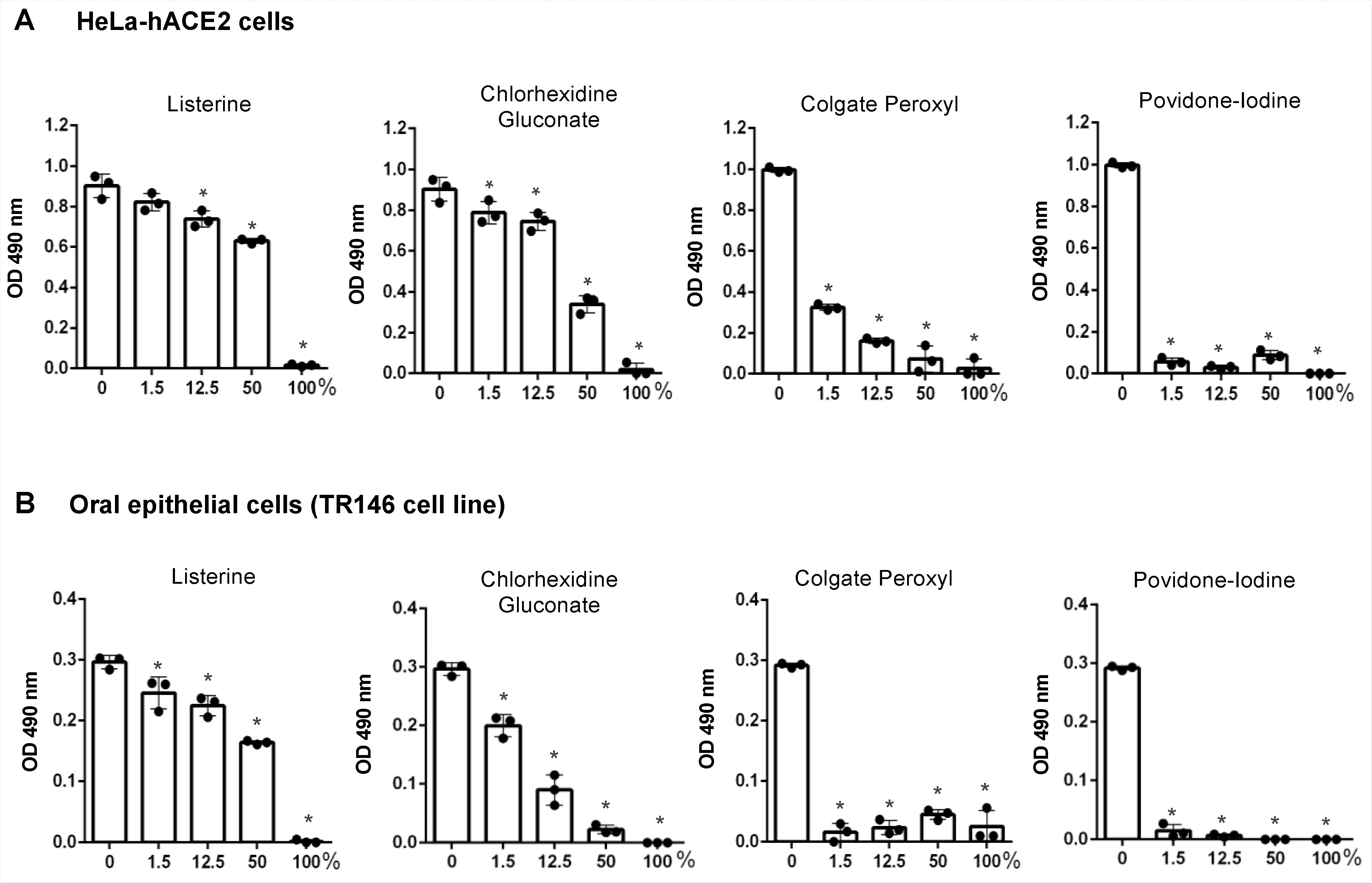
The effect of short-term exposure to mouth rinses on the viability of HeLa-hACE2 and oral epithelial cells. Human angiotensin-converting enzyme 2 (hACE2)-expressing HeLa cells (A) and oral epithelial TR146 cells (B) were treated for 20 s with different dilutions (v/v) of products including Listerine, chlorhexidine gluconate (CHG), Colgate Peroxyl, or povidone-iodine. Cells were washed and cultured with fresh medium immediately. Cell viability was determined by the 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium, inner salt (MTS)-based CellTiter 96 AQueous One Solution Cell Proliferation Assay. Data are means ±SD of three samples. The significance of differences between mouth rinse-treated cells and mocked-treated controls was compared; * p < 0.05.
"The ultimate goal would be to determine whether rinsing two or three times a day with an antiseptic agent with active anti-viral activity would have the potential to reduce the ability to transmit the disease. But this needs to be investigated in a real-world situation,'' he said.
Previous research has shown various types of antiseptic mouthwashes can disrupt the novel coronavirus and temporarily prevent transmission, but this was one of the first studies that examined antiseptic rinse concentrations, time of contact and the skin-cell killing properties that simulated oral conditions. The study was conducted by a team of dental school scientists and virologist at the Public Health Research Institute.
"Since the SARS CoV-2 virus responsible for COVID-19 enters primarily through the oral and nasal cavity, oral biologists should be included in these studies because they have an in-depth understanding of oral infectious diseases," said Fine.
Source:
Journal reference:
Xu, C., et al. (2021) Differential Effects of Antiseptic Mouth Rinses on SARS-CoV-2 Infectivity In Vitro. Pathogens. doi.org/10.3390/pathogens10030272.