Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), the causal agent of the ongoing coronavirus disease 2019 (COVID-19) pandemic, is an RNA virus belonging to the family Coronaviridae. This virus is highly virulent with a greater transmission rate and causes mild to severe symptoms. This virus has infected around 238 million individuals and claimed more than 4.8 million lives worldwide.
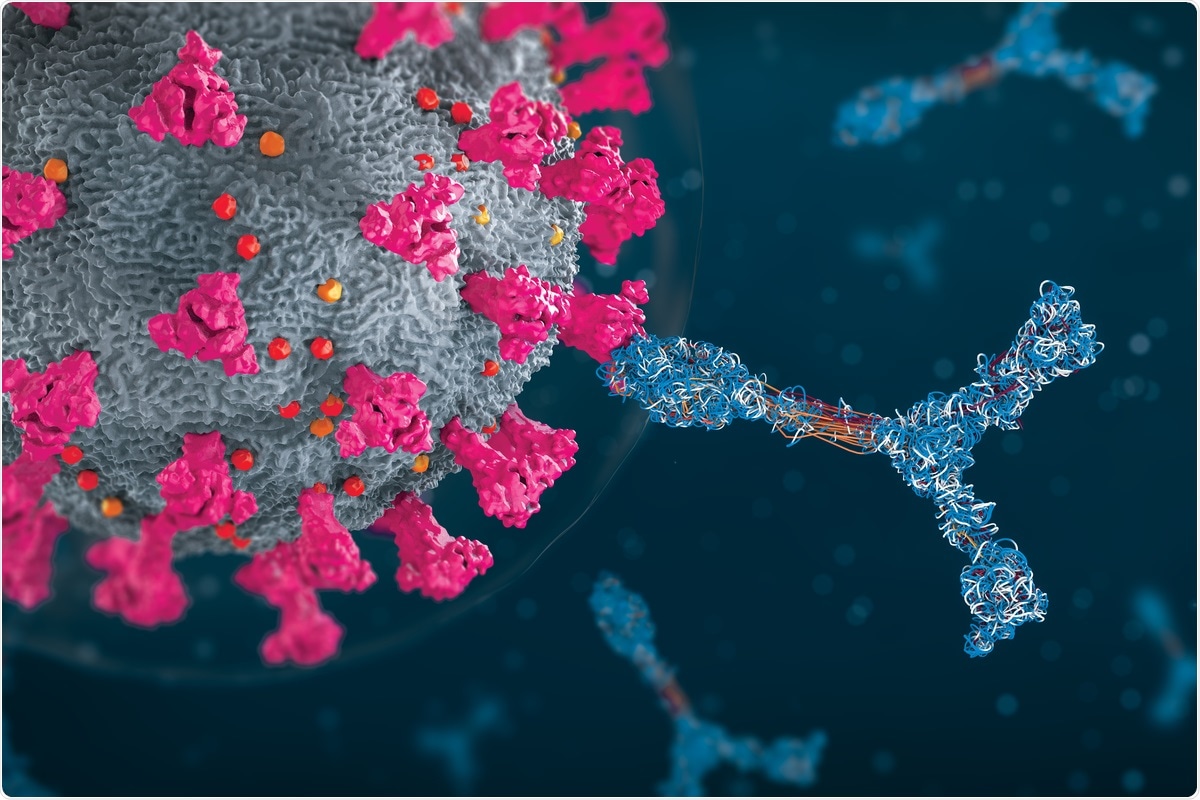 Study: Cellular and Antibody Immunity after COVID-19 Vaccination at >4-Month Follow Up in Immunocompetent and Immunocompromised Subjects. Image Credit: Christoph Burgstedt/ Shutterstock
Study: Cellular and Antibody Immunity after COVID-19 Vaccination at >4-Month Follow Up in Immunocompetent and Immunocompromised Subjects. Image Credit: Christoph Burgstedt/ Shutterstock

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Background
Several COVID-19 vaccines have been developed, and many have received emergency use authorization (EUA). In the majority of countries across the world, vaccination programs have been initiated. Owing to the emergence of SARS-CoV-2 variants due to genomic mutations, the efficacy of the approved vaccines is in question. This is because all the available vaccines have been developed against the spike protein of the original strain. Therefore, scientists have to continuously screen for new COVID-19 variants and evaluate the effectiveness of the available vaccines in managing them.
Assessment of cellular immune responses to SARS-CoV-2 is extremely important as it indicates the efficacy of vaccines against the newly emerged variants. Previous studies have revealed lower seroconversion rates after vaccination in older and immunosuppressed individuals. Many studies have reported that post-vaccination, antibodies developed in fifty percent of the total population of transplant recipients, inflammatory bowel disease patients subjected to anti-tumor necrosis factor antibodies, and individuals suffering hematologic malignancies.
Recently, scientists have characterized T-cell, B-cell, and IgG responses to S antigenic sequences to evaluate vaccine effectiveness. This study is available on the medRxiv* preprint server. In this study, scientists estimated the immune responses before and after each dose of mRNA1273 and BNT162b2 vaccines for four months in 21 healthy immunocompetent subjects. Also, samples from 20 immunocompromised (IC) subjects, vaccinated with the mRNA vaccines and Ad26.COV2.S were assessed using the same assays.
About the study
The current study revealed that after four or more months post-vaccination (first dose) in immunocompetent individuals, a decline in the receptor-binding domain (RBD)-IgG strength was observed. Additionally, a loss of the transient increase in CD8, CD4, and CD19 cell responses to the S1 antigenic sequence was reported. Interestingly, after the second dose of the COVID-19 vaccine, spike-IgG strength was stable even after the fourth month of vaccination. One of the important observations during this period was a progressive increase in S2 and S-reactive B-cells.
After the first vaccine dose, an increase in the monocytic and polymorphonuclear myeloid-derived suppressor cells (M-MDSC and PMN-MDSC) was observed. This result is in line with a previous study that reported that during the early days of COVID-19 infection, a decline in the T-cell responses to the spike protein and increased MDSC frequencies were observed. Hence, the T-cell response to vaccines reiterated the effects of COVID-19 infection.
The cellular and antibody response to S1 or its RBD component was weak and shorter-lived than Spike-IgG, which remained stable up to the fourth month. This study reported that vaccination enhanced pre-existing B-cell reactivity to the coronaviruses. Almost all the vaccinated immunocompetent subjects possessed S2-reactive B-cell frequencies in the fourth month. Sub-phenotyping of S2-reactive B-cells could determine if these cells were memory B-cells.
The current study revealed that the T-cell response appeared transient after the first dose of the COVID-19 vaccine. Researchers observed that S1-reactive T-cells reduced rapidly, while S2-reactive T-cells did not elevate above pre-vaccination levels in the four-month follow-up. One of the reasons for the decline of the suppressive effect of T-cells may be the enhancement of MDSC after the first dose of vaccination. Therefore, reducing the MDSC response to vaccination may enhance the efficacy of the vaccine.
In the cell-based assays, researchers omitted co-stimulation or the use of immunodominant peptides. This reduced the risks of overinterpreting the T-cell response to SARS-CoV-2 after vaccination of immunocompromised patients.
The authors compared the results between the immunocompetent individuals and vaccinated immunocompromised (IC) subjects for four months. There were no differences in the levels of S2-reactive T- and B-cells across the groups. Further, S1-reactive T-and B-cells were below the detectable level. Researchers of this study reported the presence of minimal numbers of S-reactive CD8+T-cells and CD19+B-cells. Among eleven IC recipients who could not produce RBD-IgG, the levels of PMN-MDSC were found to be elevated compared to immunocompetent subjects with RBD-IgG.
Conclusion
This study revealed that the SARS-CoV-2 vaccine elicits stable antibodies to neutralize spike protein. It also increases circulating B-cells reactive to the conserved spike protein sequence in immunocompetent subjects. Scientists observed that MDSC, which inhibits T- and B-cell responses, was enhanced post-vaccination. This may decrease post-vaccination immune responses, especially among IC subjects. The authors have also shown that antibody and cellular responses against SARS-CoV-2-specific spike antigenic sequences exhibited less durability.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.