
 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
The development of effective and safe COVID-19 vaccines quickly following the emergence of SARS-CoV-2 in late 2019 has been a remarkable scientific accomplishment and has lowered the number of infections and deaths associated with the disease. However, the subsequent emergence of SARS-CoV-2 variants of concern (VOCs) with a high number of mutations, including the Omicron, pose a substantial threat to public health since they significantly evade the vaccine- and natural infection-induced immunity.
The vaccine's ability to prevent infection and protect from severe outcomes such as intensive care unit (ICU) admission and mortality indicates the vaccine efficacy (VE). However, the differentiation of the impact of these two factors on VE is often challenging.
Additionally, confounding from differential testing and health-seeking behaviors based on vaccination status may skew results to show an increase in COVID-19 severity after vaccination.
About the study
In the current study, the researchers determined the impact of SARS-CoV-2 vaccination in lowering COVID-19-related ICU admission and mortality in vaccinated subjects hospitalized for COVID-19 and compared it with unvaccinated patients hospitalized with SARS-CoV-2 from January 1 to 5, 2021, in Canada.
The team utilized data from the Case and Contact Management System (CCM) of COVID-19 in Ontario, Canada, and integrated it into COVaxON, a provincial vaccination dataset, and constructed a time-matched group of subjects who were admitted to the hospital with SARS-CoV-2. The scientists only included those subjects with unique pseudo-health card numbers from the CCM to permit linkage with the COVaxON database.
Every vaccinated subject was matched up to five unvaccinated individuals based on the date of the COVID-19-positive test. The risk of COVID-19-associated ICU admission and mortality was estimated using multivariable conditional logistic regression models among the study and control groups. In addition, the factors linked to variations in vaccine effects were determined using unmatched exploratory analyses.
Study findings
The results show that among the 20,064 participants hospitalized with COVID-19 between January 1 and 5, 2021, 69.47% were aged 50 years or older, 33.41% were infected with the SARS-CoV-2 N501Y+ VOCs such as Gamma, Beta, and Alpha variants, 53.69% were males, and 21.58% had serious comorbidities. The COVID-19 vaccinated and unvaccinated participants hospitalized with SARS-CoV-2 infection demonstrated significant variations in age group, infecting SARS-CoV-2 variant, the long-term care residence, and comorbidity status in the univariable analyses.
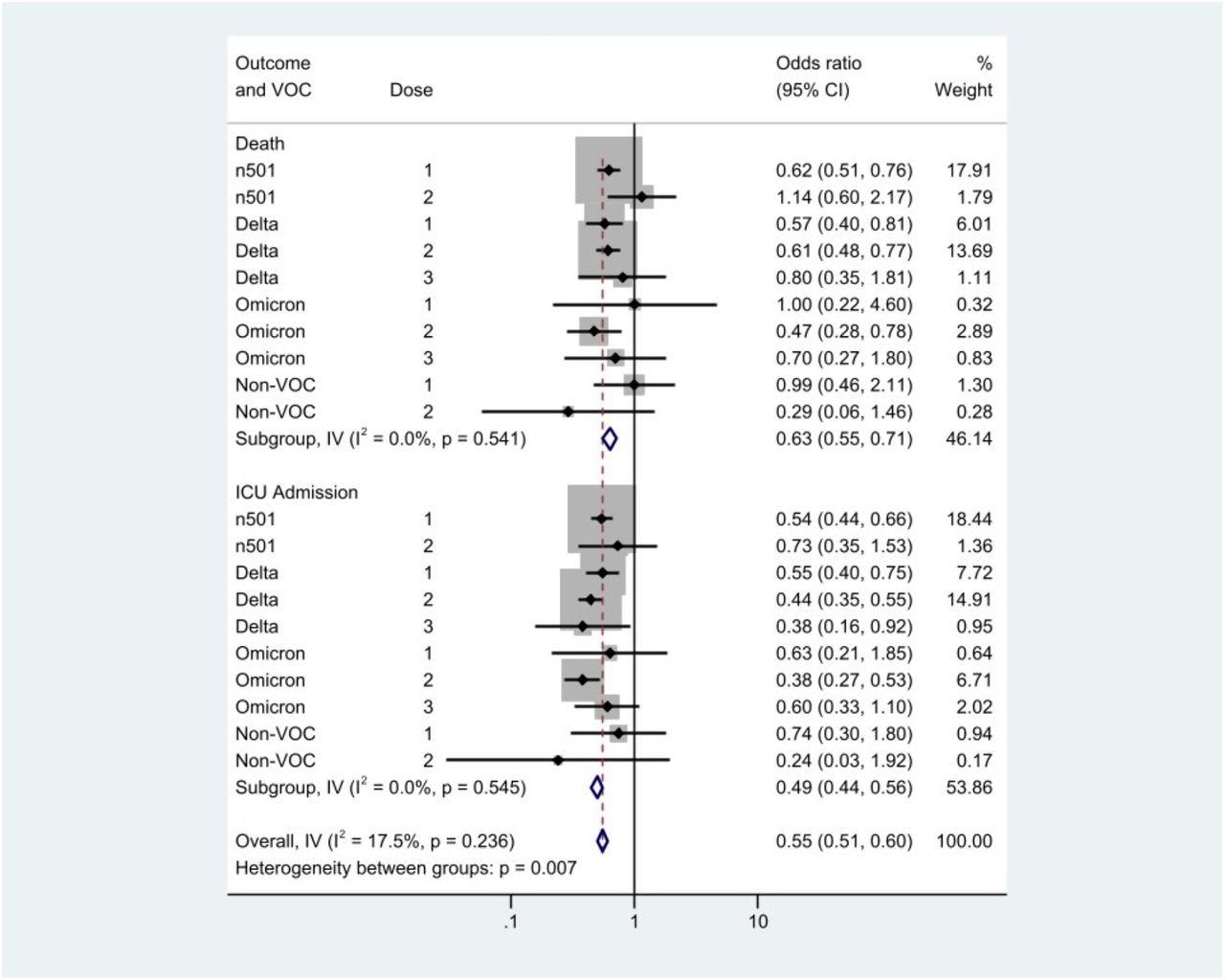
Forest plot to evaluate heterogeneity between estimates by infecting variant and outcome. The analysis is stratified by outcome, with results for death in the upper rows, and ICU admission below. NOTE: CI, confidence interval; ICU, intensive care unit; I-V, contribution of within-stratum variance to overall variance; n501, N501Y-positive variant; VOC, variant of concern.
Among the 3,353 COVID-19 vaccinated participants, 51.12%, 44.23%, and 4.65% received a single dose of vaccine, two doses, and three doses, respectively. Of the 20,064 participants hospitalized with SARS-CoV-2 infection, the 3,353 subjects who received a first, second, or third dose of COVID-19 vaccine exhibited a lower risk for SARS-CoV-2-associated ICU admission and mortality compared to the 16,711 unvaccinated individuals.
The number of SARS-CoV-2 vaccine doses received demonstrated an inverse dose-response association with the COVID-19-related ICU admission and death among the vaccinated subjects.
While the restriction analyses indicated significant vaccine-induced protection against COVID-19-related ICU admission and mortality for the SARS-CoV-2 Delta and N501Y+ variants, no relevant protection against the Omicron variant was seen, suggesting the low statistical power of the analyses because of the recent emergence of Omicron.
The risk reduction associated with COVID-19 vaccines was higher for the SARS-CoV-2-related ICU admission than the mortality in the vaccinated lot. Nonetheless, no substantial variation in risk for infection with SARS-CoV-2 VOCs was observed among the vaccinated and unvaccinated participants.
Conclusions
The study findings implied a lower risk of COVID-19-related ICU admission and mortality in hospitalized SARS-CoV-2-vaccinated subjects than the time-matched unvaccinated controls in Ontario, Canada. Nevertheless, the COVID-19 vaccines failed to prevent a severe SARS-CoV-2 infection that required hospitalization. COVID-19 vaccines remain an essential technique for reducing ICU admission and death in COVID-19, despite their reduced effectiveness against novel SARS-CoV-2 VOCs infections. Hence, higher SARS-CoV-2 vaccination rates are required to protect community health and lower mortality and the requirement of the ICU during the ongoing COVID-19 pandemic.
A significant limitation of the present study was the inability to confirm that the results seen were not at least in part attributable to residual confounding, suggesting future studies are warranted to overcome this limitation. Further, the study lacked statistical power to evaluate Omicron-specific protections associated with vaccines due to the recent emergence of the variant and the delay in progression to serious COVID-19 and death.
Overall, the study emphasizes that COVID-19 vaccination is of paramount significance to healthcare systems and individuals even when it fails to prevent SARS-CoV-2 infection and hospitalization as it reduces SARS-CoV-2-related ICU admissions and mortality rates.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Relative Virulence of SARS-CoV-2 Among Vaccinated and Unvaccinated Individuals Hospitalized with SARS-CoV-2, Alicia A. Grima, Kiera R. Murison, Alison E. Simmons, Ashleigh R. Tuite, David N. Fisman, medRxiv 2022.02.15.22271016; doi: https://doi.org/10.1101/2022.02.15.22271016, https://www.medrxiv.org/content/10.1101/2022.02.15.22271016v1
- Peer reviewed and published scientific report.
Grima, Alicia A, Kiera R Murison, Alison E Simmons, Ashleigh R Tuite, and David N Fisman. 2022. “Relative Virulence of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) among Vaccinated and Unvaccinated Individuals Hospitalized with SARS-CoV-2.” Clinical Infectious Diseases, May. https://doi.org/10.1093/cid/ciac412. https://academic.oup.com/cid/article/76/3/e409/6591845.