Various case and hospital-based studies have shown a high risk of venous thromboembolism (VTE) in patients with severe coronavirus disease 2019 (COVID-19). More specifically, a pooled VTE rate of 14.7% and 23.2% was reported in a recent meta-analysis among patients who were admitted to the hospital and intensive care units (ICUs), respectively.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Background
Several randomized controlled trials have also demonstrated the benefit-risk of anticoagulation therapy for COVID-19 patients who were at different stages of the disease. Despite these findings, there remains a lack of recommended interventions for the prevention of VTE amongst ambulatory patients with COVID-19.
The global rollout of vaccines, the widespread transmission of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Omicron variant, and the relaxation of public health restrictions have caused an increase in the number of milder COVID-19 cases that are managed in ambulatory settings. Simultaneously, the lack of insight regarding the impact of clinical, genetic, and socio-economical risk factors on infection-related VTE has persisted.
A new study published on the preprint server medRxiv* aims to quantify the risk of acute VTE due to SARS-CoV-2 infection in ambulatory settings, as well as identify the clinical and genetic risks of VTE determinants following SARS-CoV-2 infection.
About the study
The current study included U.K. Biobank (UKBB) participants from England who were alive on March 1, 2020. Study participants were divided into an infected cohort and a non-infected cohort.
Participants who tested positive for COVID-19 by polymerase-chain-reaction (PCR) assay between March 1, 2020, and September 30, 2021, were included in the infected cohort, while participants who never tested or only had negative test results were included in the non-infected cohort.
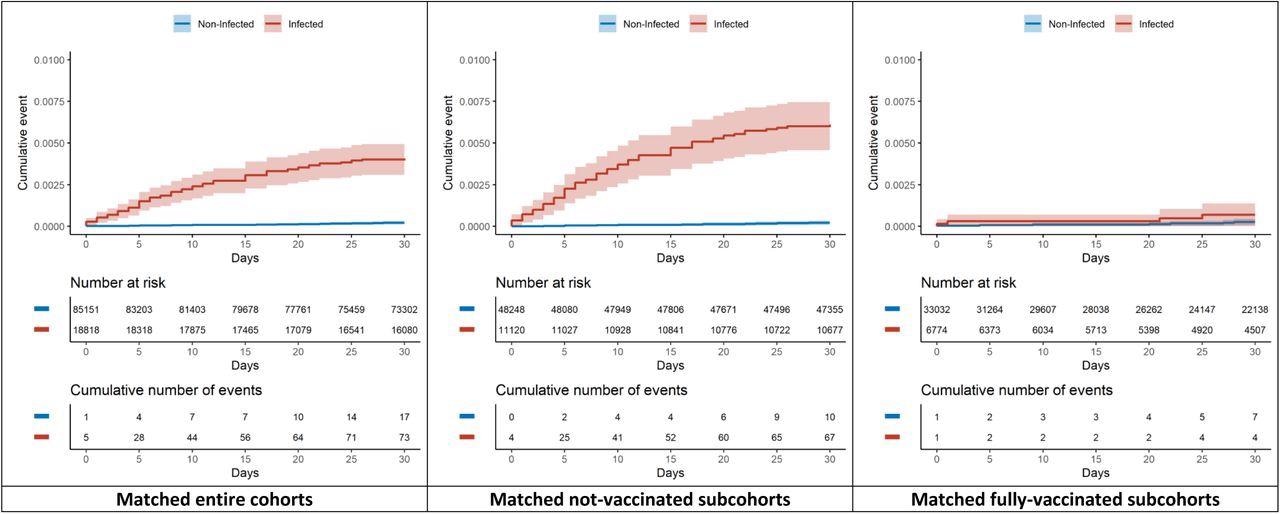
Cumulative incidence curves of venous thromboembolic events within 30 days.
Thereafter, an index date was defined as the date of the first positive specimen sample for the infected cohort and a random date during the same period for the matched non-infected cohort. Participants who used antithrombotic drugs one year before index dates with historical VTE, as well as those who tested positive in hospital settings, were excluded from the study.
Inherited thrombophilia carriers were defined as those with two risk single nucleotide polymorphisms (SNPs) in Factor V Leiden or Prothrombin G20210A. A 297-SNPs polygenic risk score (PRS) was also calculated for VTE that did not include these two variants.
A list of co-variates was studied such as demographics, body mass index (BMI), socio-economic status, comorbidities, vaccination status, number of hospitalizations in the last one year, and medications taken before one year of the index date. Participants were followed up for 30 days after the index date for the occurrence of incident VTE comprising either deep vein thrombosis or pulmonary embolism.
Study findings
Out of the 407,311 UKBB participants, 26,210 were infected with SARS-CoV-2 during the study period. After applying the exclusion criteria, 83% of infected participants and 78.23% of non-infected participants were included in the study. Of the infected participants, 13% were tested in hospitals, and 87% were tested in outpatient settings.
Ambulatory COVID-19 patients were found to be younger than the uninfected, from non-White ethnicity, and more likely to be male, obese, and more socioeconomically deprived. A total of 73 and 17 VTE events were observed among ambulatory patients and matched uninfected within the 30 days follow-up period, respectively. Furthermore, SARS-CoV-2 infection was associated with an increased risk of VTE, especially in unvaccinated participants.
Men, older participants, and people who were obese were at a higher risk of COVID-19-associated VTE, while a two-dose vaccination was associated with a lower risk of COVID-19-related VTE.
Out of all the infected participants, 1,287 had inherited thrombophilia with 392 carrying the risk variant of Prothrombin G20210A and 909 carrying the risk variant of Factor V Leiden. Participants with inherited thrombophilia were at a higher risk of VTE following SARS-CoV-2 infection as compared to those without. However, no association was found between inherited thrombophilia and arterial thromboembolism.
Conclusions
The current study demonstrates that ambulatory COVID-19 was associated with a 20-fold increase in incident VTE; however, no elevated risk was observed in fully vaccinated individuals. Several factors such as sex, older age, and obesity could increase the risk of COVID-19 related VTE.
Additionally, inherited thrombophilia was found to double the risk of COVID-19 related VTE. Therefore, high vaccine coverage and targeted strategies are required to prevent VTE during the outpatient care of COVID-19.
Limitations
The current study was not free from residual confounding. Additional limitations included that the study population could not fully represent the general population and that the association of asymptomatic infection with VTE risk was not assessed. Finally, the estimates of the study were an average and mixed effect of several SARS-CoV-2 strains.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Xie, J. Q., Prats-Uribe, A., Feng, Q., et al. (2022). Venous Thromboembolism in Ambulatory Covid-19 patients: Clinical and Genetic Determinants. medRxiv. doi:10.1101/2022.03.22.22272748. https://www.medrxiv.org/content/10.1101/2022.03.22.22272748v1.
- Peer reviewed and published scientific report.
Xie, JunQing, Albert Prats-Uribe, Qi Feng, YunHe Wang, Dipender Gill, Roger Paredes, and Dani Prieto-Alhambra. 2022. “Clinical and Genetic Risk Factors for Acute Incident Venous Thromboembolism in Ambulatory Patients with COVID-19.” JAMA Internal Medicine, August. https://doi.org/10.1001/jamainternmed.2022.3858. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2795466.