Several studies, including exogenous peptide assays, have demonstrated how mutations within SARS-CoV-2 epitope sequences lead to viral escape from T cell responses. In addition, for human immunodeficiency virus (HIV-1), studies have evidenced that these mutations disrupt proteasomal cleavage. However, the effects of SARS-CoV-2 epitope-flanking mutations on viral epitope antigen processing and CD8+ T cell activation are currently unknown.
About the study
In the present study, researchers searched sequences of two immunodominant SARS-CoV-2 NP epitopes - NP9- 17 and NP105-113. They identified 29 mutations in the flanking regions, i.e., within six amino acids on either side of the epitopes. They used stable B cell lines expressing SARS-CoV-2 wild-type (wt) or mutated NP through lentiviral transduction for the evaluation. Likewise, the researchers assessed these sequences using the NetChop 20S 3.0 prediction tool to predict proteasomal cleavage sites in both wt and mutated NP sequences.
Each NP construct contained a green fluorescent protein (GFP) gene separated by a viral self-cleavage T2A site, resulting in one long transcript and two translated proteins, GFP and NP. They used the mutation NP-P13L as a control because it is a CD8+ T cell escape mutant within the epitope NP9-17.
Notably, the team retrieved sequence data from the Global Initiative On Sharing The Avian Influenza Data (GISAID) database.
The team selected seven mutations that showed the most significant predicted differences in proteasomal cleavage compared to the wt NP sequence for each epitope for further investigations.
The researchers tracked the frequency of mutations over time using a mutation tracking tool. Additionally, they performed flow cytometry analysis of transduced B cells for which they co-cultured bulk CD8+ T cells specific for NP9-17 or NP105-113 for four hours before analysis of CD107a interferon-gamma (IFN-γ), and tumor necrosis factor (TNF)-α expressions.
Further, to demonstrate the differences in CD8+ T cell responses, the researchers used a 2:1 to 0.1:1 range of effector (CD8+ T cell) to target (NP-transduced B cell) ratio (E: T).
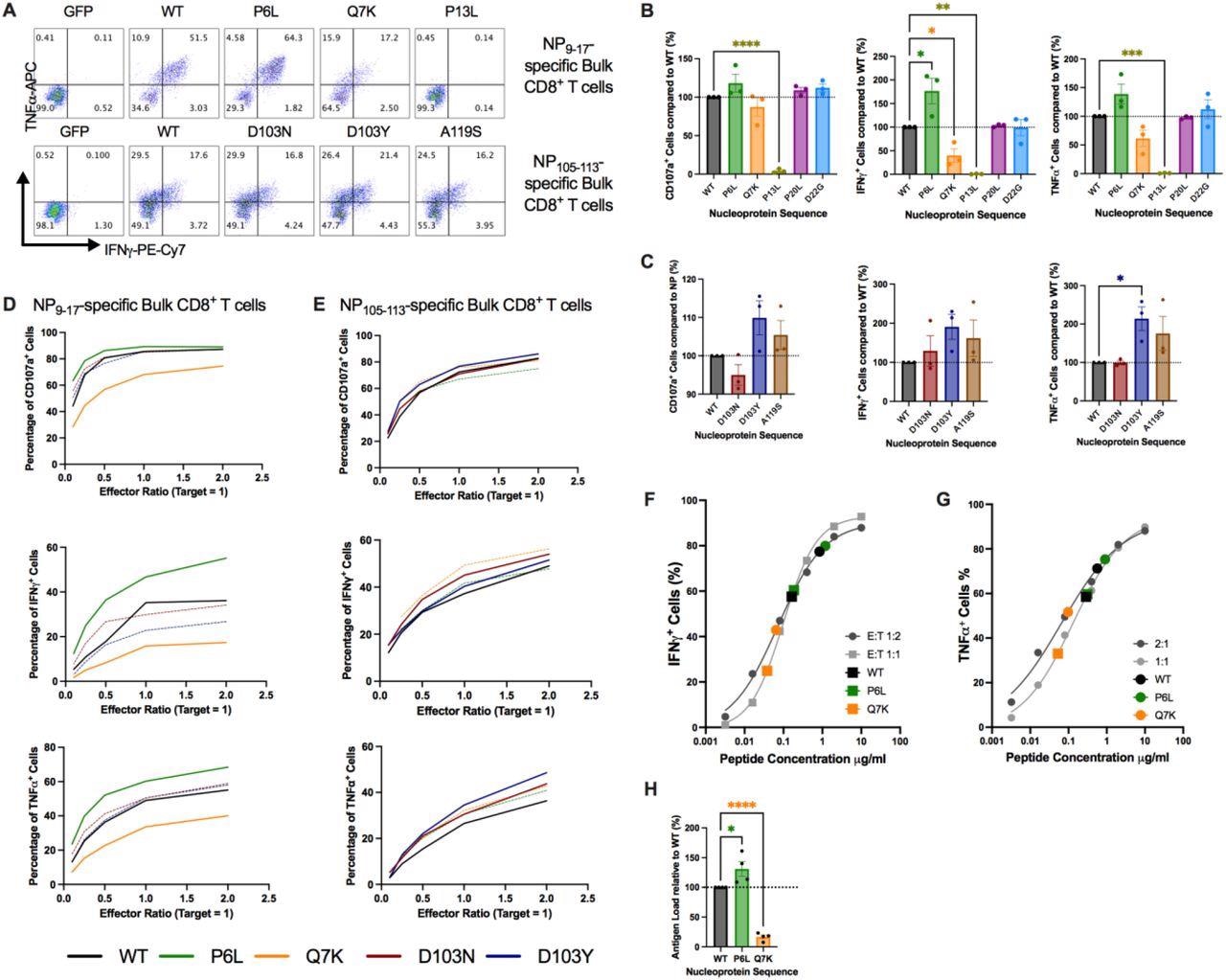
Mutations in flanking regions of epitopes alter CD8+ T Cell responses, (A) Intracellular cytokine staining of NP9-17 or NP105-113 epitope-specific bulk CD8+ T cells following incubation with GFP-or NP-transduced B cells. (B) CD8+ T Cell responses to mutations flanking NP9-17 were analyzed by flow cytometry at an E:T ratio of 2:1. (C) CD8+ T Cell responses to mutations flanking NP105-113 were analyzed by flow cytometry at an E:T ratio of 2:1. (D-E) Selected mutations were investigated in more detail by altering the E:T ratio from 2:1 to 0.1:1. (F) IFNγ titration curve in response to NP9-17 epitope peptide for NP9-17-specific bulk CD8+ T cells with NP-transduced B cell responses overlaid. (G) TNFα titration curve in response to NP9-17 epitope peptide for NP9- 17-specific bulk CD8+ T cells with NP-transduced B cell responses overlaid. (H) Estimated peptide load values were normalized to WT-NP levels. Data is presented as mean ±SEM and was analyzed by one-way ANOVA and Dunnett’s multiple comparisons test. *p<0.05, **p<0.01, ***p<0.001, ****p<0.0001.
Study findings
Although the mutations examined in the present study are not currently present in any SARS-CoV-2 variants, their frequency has been rising since July 2020. Accordingly, despite the early time point of sequence sampling, three of the 29 identified mutations (10%) showed significant differences in the CD8+ T cell responses.
In particular, four mutations showed differences in the amount of 9-mer epitope peptides when investigated for their effect on proteasomal digestion, thus indicating that the epitope flanking regions have many naturally-occurring mutations that can potentially alter T cell responses.
NP-transduced cells showed no significant differences in GFP, SARS-CoV-2 NP, or human leukocyte antigen (HLA) expression. However, for the mutations flanking NP9-17, there was a distinct separation between the wt vs. mutant results, with the NP-Q7K showing lower and the NP-P6L showing higher T cell responses. For NP105-113, the differences were slightly restrained, but again there was a separation between wt and mutant protein results.
Taken together, the study results demonstrated that flanking mutations, particularly in the N-terminal mutants, significantly altered CD8+ T cell responses, for which the mutations most likely altered the antigen load of the epitopes on the cell surface.
Interestingly, the NP9-17 epitope showed the greatest differences across the range of E: T ratios examined during the study. The authors also observed diminished CD8+ T cell responses to the NP-Q7K mutation by NP9-17-B*27:05 epitope, which was linked with lower epitope surface expression. An inefficient epitope production by proteasome indicated immune evasion capabilities conferred by the NP-Q7K mutation. Contrastingly, the NP-D103N/Y and NP-P6L mutations flanking the NP9-17-B*27:05 epitopes and NP105-113-B*07:02, respectively, increased CD8+ T cell responses linked to augmented epitope production by the proteasome.
To summarize, the study identified the beneficial natural mutations within SARS-CoV-2 immunodominant T cell epitope flanking regions that had a remarkable potential to boost antigen processing and effectiveness of T cell recognition, thus opening new possibilities for research for coronavirus disease 2019 (COVID-19) vaccine design.

 *Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Journal reference:
- Preliminary scientific report.
SARS-CoV-2 mutations affect proteasome processing to alter CD8+ T cell responses, Dannielle Wellington, Zixi Yin, Zhanru Yu, Raphael Heilig, Simon Davis, Roman Fischer, Suet Ling Felce, Philip Hublitz, Ryan Beveridge, Danning Dong, Guihai Liu, Xuan Yao, Yanchun Peng, Benedikt M M Kessler, Tao Dong, bioRxiv 2022, DOI: https://doi.org/10.1101/2022.04.08.487623, https://www.biorxiv.org/content/10.1101/2022.04.08.487623v1