Snoring, which happens when the soft tissue in the upper airway narrows and vibrates, is a common phenomenon thought to occur in up to 83% of men and 71% of women. It has been associated with partial obstruction of airways, sleep apnea, and damage to surrounding areas such as carotid arteries.
Snoring may also be an indication of high blood pressure and lead to poor sleep quality, thus increasing the risk of hypertension. Researchers have raised concerns about using self-reported data or short-term observations to assess health risks associated with snoring. Recent technological advancements allow for home-based monitoring strategies to be integrated into research and provide important insights into the relationships between snoring and health.
About the study
People who registered to use a sleep sensor placed under their mattresses and a home-based blood pressure monitor from July 2020 to April 2021 were included in the study. The sensor generated an estimated apnea-hypopnea index (eAHI), detected snoring, and identified stages of sleep using proprietary algorithms. Blood pressure was collected from the measurements taken using the blood pressure monitor by the participants.
Mean snoring duration and mean eAHI were the exposure variables used in the analysis, which included linear and logistic regressions and the calculation of odds ratios but also addressed the possibility of non-linear associations using restricted cubic splines. Interactions with BMI, sex, and age were considered. Sensitivity analyses adjusted the initial models with total time spent sleeping and accounted for within-day blood pressure variation.
Findings
A total of 12,287 people were included in the study, with the average participant aged 50 years and overweight with a body mass index (BMI) of 28 kg/m2. Nearly 90% of the participants were male. For each individual, a median of 29 blood pressure recordings and 181 sleep and snoring recordings on average were collected.
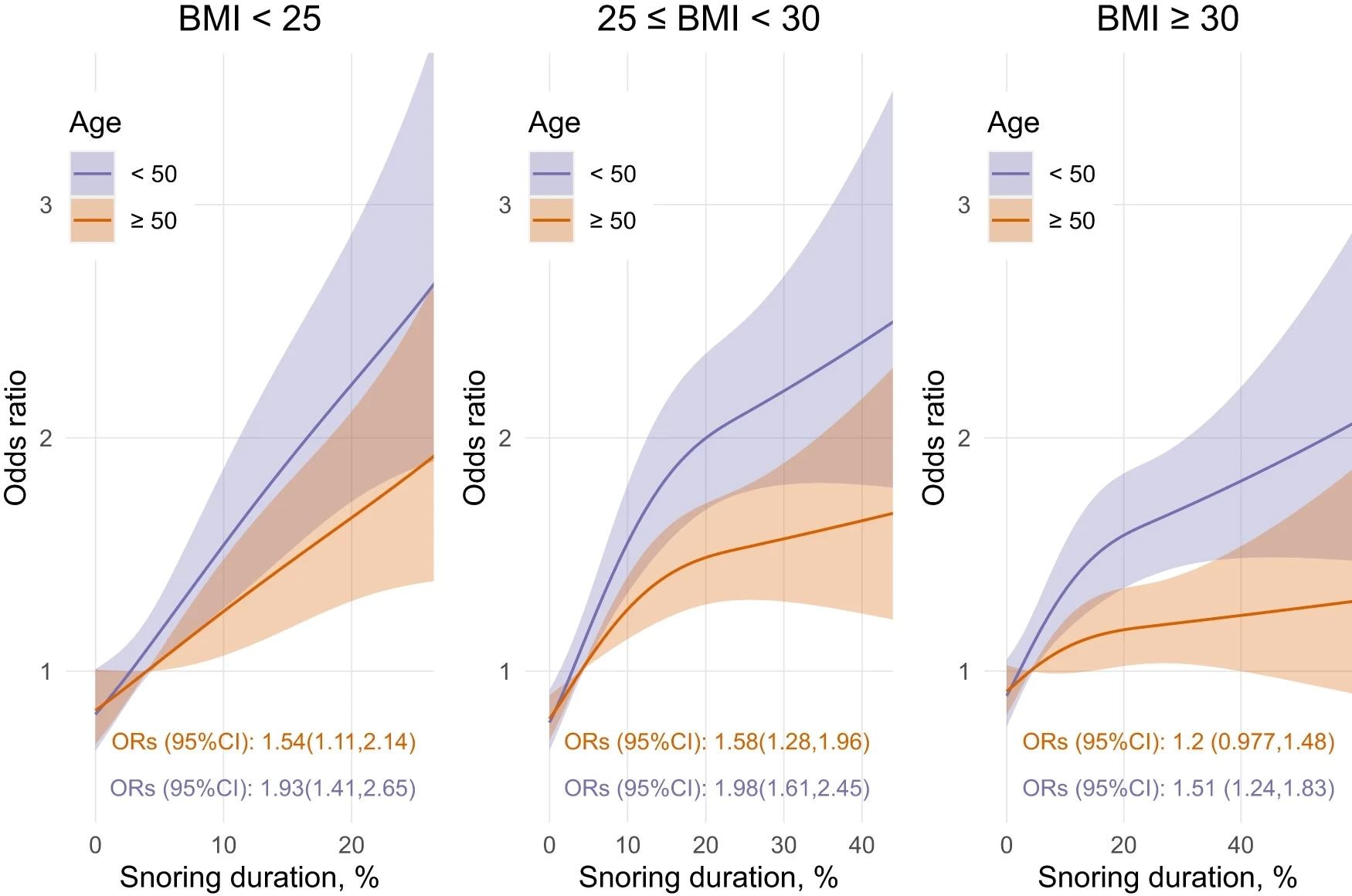 Models use 3 knots restricted cubic spline and interaction with age categories (median split in years) and BMI categories (kg/m2). ORs (95%CI) represents the difference between the 5% and the 75% percent of the snoring duration distribution. Note that the 5% and 75% percent were determined separately for each BMI category; hence, slightly different x-axis.
Models use 3 knots restricted cubic spline and interaction with age categories (median split in years) and BMI categories (kg/m2). ORs (95%CI) represents the difference between the 5% and the 75% percent of the snoring duration distribution. Note that the 5% and 75% percent were determined separately for each BMI category; hence, slightly different x-axis.
Nearly half of the participants snored for more than 5% of the night, but only 7% spent more than 30% of the night snoring; time spent snoring was higher for men than women. The correlation coefficient between the eAHI and snoring duration was 0.42, and people with obstructive sleep apnea (OSA) spent more time snoring on average than those without the condition.
After adjusting for sex, eAHI, and BMI, people who snored longer had higher diastolic and systolic blood pressure by 3-4 mmHg on average. The effect sizes of interactions with age and obese status were small, though significant.
Participants who did not have OSA but had high snoring levels had a 3.8 mmHg higher systolic blood pressure and 4.5 mmHg higher diastolic blood pressure than those who did not snore or have sleep apnea. The effect of snoring without OSA on blood pressure was comparable to that of OSA without snoring on blood pressure.
The duration of snoring was significantly correlated with uncontrolled hypertension, regardless of sex, though associations were stronger for people with a BMI<30 and less than 50 years old. People less than 50 years old with a normal BMI showed an increase in hypertension likelihood of 98% if they snored.
In sensitivity analyses, researchers adjusted for the total time spent asleep, but this did not significantly affect their findings. For example, models that adjusted for sleep time found that higher snoring duration was associated with an 88% rise in uncontrolled hypertension.
Conclusions
The findings indicate that snoring regularly at night is strongly associated with high blood pressure and uncontrolled hypertension, regardless of the presence or severity of OSA, especially among middle-aged and overweight men who made up the majority of the studied population. The authors recommend that snoring be considered a part of the clinical care of sleep-related problems and hypertension management.
This study overcomes certain limitations of previous explorations in this field, which relied either on self-reported snoring data or recordings from a single night and were thus unable to account for night-to-night variability. However, the study did not assess confounding factors such as the use of alcohol, tobacco, and caffeine, diet, medications, and exercise.
Findings from the predominantly male, obese, and middle-aged population cannot be generalized to other groups. Another important consideration is that people more concerned about their health are more likely to register to use the devices, potentially confounding the findings. Further studies can focus on addressing these issues and strengthen the evidence base on this topic.
Journal reference:
- Regular snoring is associated with uncontrolled hypertension. Lechat, B., Naik, G., Appleton, S., Manners, J., Scott, H., Nguyen, D.P., Escourrou, P., Adams, R., Catcheside, P., Eckert, D.J. npj Digital Medicine (2024). 10.1038/s41746-024-01026-7, https://www.nature.com/articles/s41746-024-01026-7