A new clinical study reveals that daily black tea kombucha can promote healthier gut bacteria, especially in people with obesity, by reducing harmful microbes and supporting beneficial ones.
 Homemade black tea kombucha. Image Credit: Ildi Papp / Shutterstock. Study: Regular Consumption of Black Tea Kombucha Modulates the Gut Microbiota in Individuals with and without Obesity
Homemade black tea kombucha. Image Credit: Ildi Papp / Shutterstock. Study: Regular Consumption of Black Tea Kombucha Modulates the Gut Microbiota in Individuals with and without Obesity
In a recent study in The Journal of Nutrition, researchers investigated the intestinal health impacts of regular black tea kombucha. The study was carried out over eight weeks and comprised initially 46 participants, with 23 participants assigned to each of two categories: normal weight or obese. Ultimately, 38 participants completed the study. Study outcomes were measured by comparing participants’ stool, urine, and blood samples between baseline (0 weeks) and completion (8 weeks of intervention).
Study findings revealed that the kombucha contains 145 phenolic compounds (flavonoids = 81%, phenolic acids = 19%) and contributes to the growth of beneficial gut bacteria across both cohorts. The obesity groups derived the most benefit, with regular kombucha consumption resulting in the growth of the butyrate producer Subdoligranulum and declines in obesity-associated genera like Ruminococcus and Dorea. Changes in gut fungal composition were also observed after the kombucha intervention, with an increase in the abundance of certain fungi like Saccharomyces, though overall fungal alpha-diversity did not generally increase across all groups and was noted to be higher at baseline in the obese group before potentially decreasing or changing by the end of the intervention.
Background
Obesity is a growing global health concern, afflicting more than 1 billion people today, and estimates expect this prevalence to increase further in the coming years. Decades of research have revealed environmental, genetic, physiological, and behavioral influences in the manifestation and progression of obesity, but the mechanisms underpinning these interactions remain poorly understood. A growing body of literature highlights the close relationship between gut microbiome health and optimal lipid outcomes, with dysbiosis of the former often triggering obesity in the host.
Diet's impacts on gut health and obesity cannot be understated. Recent research suggests that what we eat can modulate our weight and determine the composition and structure of the microorganisms inhabiting our guts. Kombucha, a fermented beverage produced when a Symbiotic Culture of Bacteria and Yeast (SCOBY) is grown on tea infusions, has received increasing scientific and media attention given its dietary health benefits.
These benefits are especially relevant in gut microbial research, where animal models have repeatedly validated the modulatory effects of the phenol-rich beverage on the gut microbiome. Unfortunately, no studies have yet confirmed these findings in humans.
About the study
The present study aims to address this knowledge gap by investigating the long-term (eight weeks) impacts of consistent black-tea kombucha consumption on gut microbial health and assessing how these impacts differ between participants with and without obesity. The study measured gut microbiota changes, short-chain fatty acid (SCFA) content, and intestinal permeability of all participants at study enrolment and intervention termination. It's important to note that this study used a pre-post intervention design without a parallel control group that did not consume kombucha.
Prospective participants were recruited through institutional emails and social media advertisements and were required to undergo questionnaire-based screening before study enrolment. Participants between the ages of 18 and 45, with a body mass index (BMI) value of at least 18.5 kg/m2, and devoid of a medical history of chronic diseases (except obesity) were enrolled.
Excluded were those who consumed kombucha (at least once a week over the past month); regularly used anti-inflammatory drugs, corticoids, or drugs that affect lipid or glucose metabolism; used antioxidant or vitamin supplements; took antibiotics 3 months before the study; had infectious or allergic episodes in the last month; were on weight loss diets; did not present a stable weight over the 3 months before the study (±3 kg); had an aversion to kombucha; had alcohol intake greater than 105 g of ethanol/week for women and 210 g for men; smokers; and pregnant and lactating women.
All participants were subjected to a baseline evaluation, which included collecting demographic data, medical records, laboratory examinations, and biological samples (blood, stools, and urine).
The study intervention involved the distribution of laboratory-prepared black tea kombucha (200 mL) for daily consumption. Simultaneous food frequency questionnaires (FFQs) and the International Physical Activity Questionnaire (IPAQ) were maintained to ensure that participants did not significantly alter their routine diets and physical activity levels.
Researchers used a combination of titration, high-performance liquid chromatography (HPLC), ultra-performance liquid chromatography mass spectrometry (UPLC-MS), and Folin–Ciocalteu colorimetric assays to characterize the composition of their black-tea kombucha. Microbiological characterization (serial dilution approach), intestinal permeability (lactulose and mannitol), and biomarker identification (ELISAs) helped elucidate the impacts of consistent kombucha consumption on the gut.
Study findings
Of the 193 online respondents, 62 were screened, of which 46 participants (25 female) were enrolled after having met all inclusion criteria. Participants were equally divided between the ‘normal weight’ (mean BMI = 21.64 kg/m2) and ‘obese’ (mean BMI = 34.47 kg/m2) cohorts (n = 23 each). Laboratory-generated black-tea kombucha presented with a low pH (increased acidity) and a residual slightly sweet taste (sugar added for fermentation).
The IPAQ results showed that, at baseline, 61.1% of participants were active, 16.7% were very active, 5.6% were irregularly active A, and 16.7% were irregularly active B. After 8 weeks of kombucha consumption, physical activity patterns remained mostly unchanged, with only 3 participants showing a shift, 2 in the normal weight group and 1 in the obese group.
UPLC-MS-based characterization of the kombucha revealed it to be a rich source of phenolic compounds (n = 145), including flavonoids (81%) and phenolic acids (19%). Quercetin 3-O-rutinoside was found to be the most abundant phenol in the beverage. Frequent kombucha consumption was found to promote the growth of commensal Bacteroidota and Akkermanciaceae bacteria, with bacterial growth strongest in obese participants.
Obese participants also benefited from an increase in Subdoligranulum (butyrate producer) populations and significant reductions in Ruminococcus and Dorea (obesity-associated) genera. Encouragingly, Ruminococcus and Dorea levels, which were significantly higher in the obese cohort compared to normal-weight participants, were reduced in the obese participants to normal baseline levels by intervention termination. However, the study did not find significant differences in short-chain fatty acid (SCFA) concentrations (acetate, butyrate, and propionate) in the stool samples of participants in either group, before or after the 8-week kombucha consumption. Similarly, markers of intestinal permeability, such as the lactulose to mannitol ratio in urine and plasma zonulin concentrations, did not show significant changes between or within groups after the intervention.
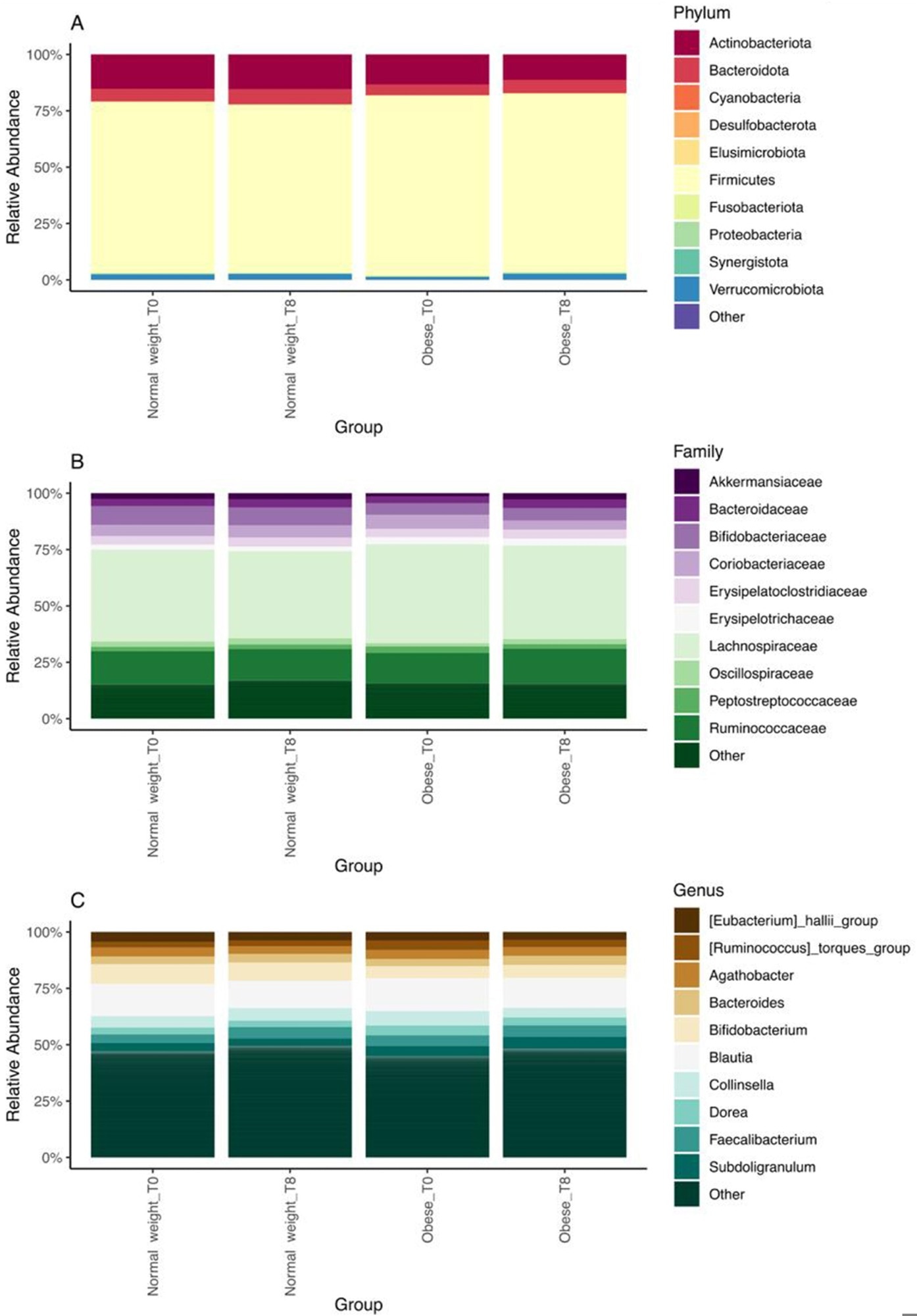
Relative abundance of major phyla (top 10) (A), families (top 10) (B), and genera (top 10) (C) in normal weight and obese groups at baseline (T0) and after 8 wk of regular consumption of black tea kombucha (T8).
Conclusions
The present study establishes the beneficial gut microbial effects of frequent kombucha consumption, particularly in obese or overweight individuals who experience greater benefits than their normal-weight counterparts in terms of bacterial modulation. Kombucha was observed to be a rich source of beneficial phenols (n = 145), some of which have known anti-obesity benefits. While the intervention led to these positive shifts in gut bacteria and fungal composition, it's noteworthy that direct measures of short-chain fatty acid production in stool and markers of intestinal permeability did not significantly change within the 8-week study period. Future research with a control group and potentially longer intervention durations would be beneficial to confirm these findings and explore potential clinical impacts.
Regular kombucha consumption positively influenced gut microbiota in both normal and obese groups, with more pronounced effects in the obese group, suggesting that it may be especially beneficial for those individuals.
Journal reference:
- Costa, M. A. de C., da Silva Duarte, V., Fraiz, G. M., Cardoso, R. R., da Silva, A., Martino, H. S. D., dos Santos D’Almeida, C. T., Ferreira, M. S. L., Corich, V., Hamaker, B. R., Giacomini, A., Bressan, J., & Barros, F. A. R. de. (2025). Regular Consumption of Black Tea Kombucha Modulates the Gut Microbiota in Individuals with and without Obesity. The Journal of Nutrition, 155(5), 1331–1349, DOI: 10.1016/j.tjnut.2024.12.013, https://www.sciencedirect.com/science/article/pii/S0022316624012392