While GLP-1 receptor agonists like semaglutide help with weight loss, new research shows users often fall short on vital nutrients, spotlighting the urgent need for tailored dietary guidance.
 Study: Investigating nutrient intake during use of glucagon-like peptide-1 receptor agonist: a cross-sectional study.
Study: Investigating nutrient intake during use of glucagon-like peptide-1 receptor agonist: a cross-sectional study.
In a recent study published in the journal Frontiers in Nutrition, researchers examined nutrient intake when using a glucagon-like peptide 1 receptor agonist (GLP-1RA). Obesity prevalence has doubled since 1990, with one in eight individuals being obese worldwide. Recent pharmaceutical interventions, especially GLP-1RAs, have advanced treatment for glycemic control and obesity. Notably, GLP-1RAs slow the transit time of the gastrointestinal (GI) tract and suppress appetite, which could displace nutrient intake and result in mineral and vitamin deficiencies.
Besides, side effects could interfere with food preferences, leading to suboptimal intake of specific foods. As such, optimal health outcomes with GLP-1RA require a multifaceted approach beyond pharmacological interventions, encompassing lifestyle modifications like diet and exercise. However, limited or no medical nutrition therapy (MNT) guidelines are provided to healthcare providers and patients regarding adequate nutrient intake during GLP-1RA use.
About the study
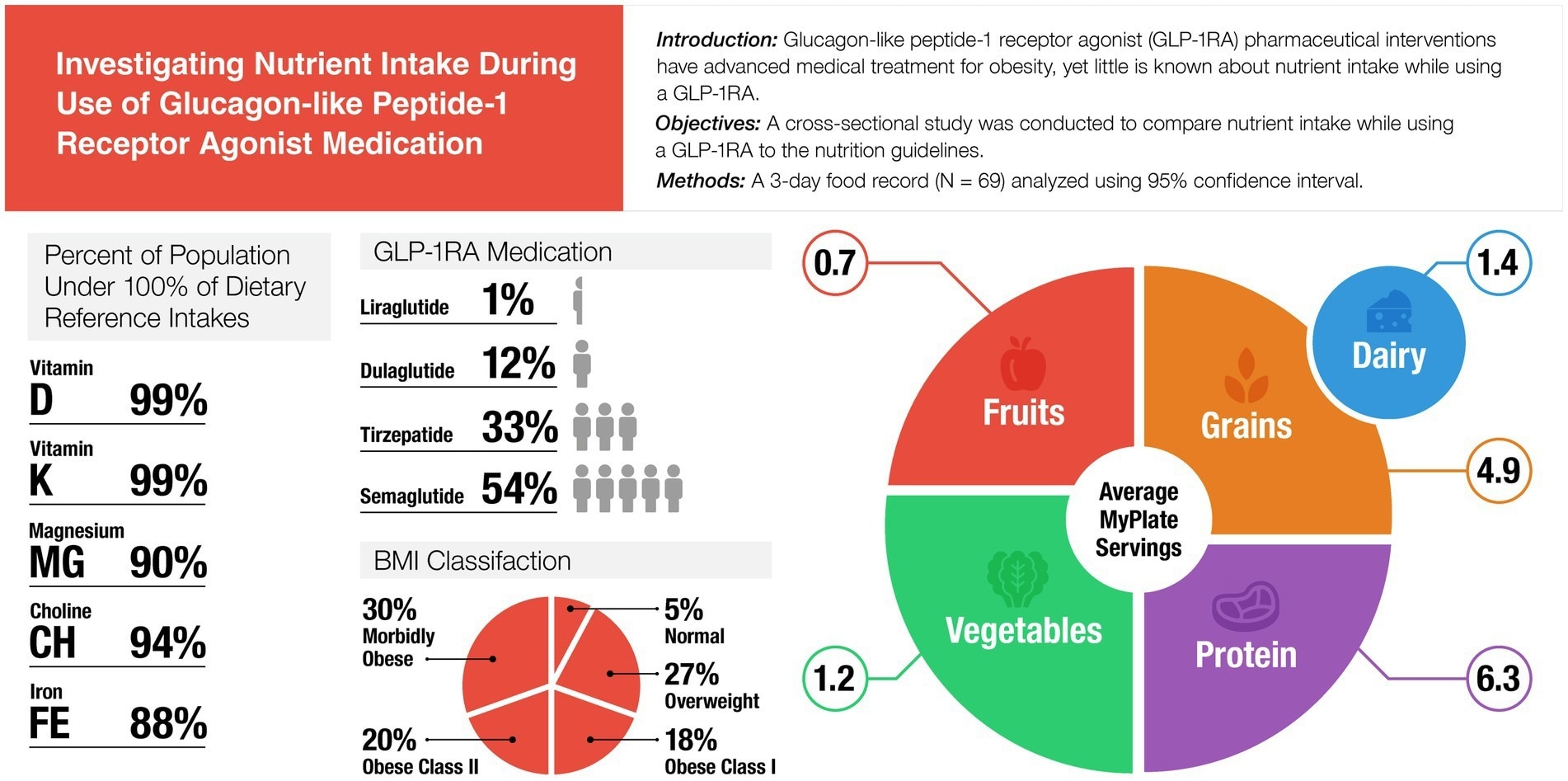
The present study compared the nutrient intakes of GLP-1RA users to dietary reference intakes (DRI). Between September and October 2024, adults aged ≥ 18 years or older who had used a GLP-1RA for at least a month were recruited. Individuals enrolled in other nutrition programs or receiving meal plans were excluded. Self-reported questionnaires for anthropometrics, demographics, dietary habits, and GLP-1RA usage were administered.
Participants were asked about the education they received from healthcare providers during prescription and the level of satisfaction with that information. They were also asked about GLP-RA use, including the specific drug, reasons for use, duration, side effects, and expected period of future use. Participants self-reported general dietary habits, including changes in food preferences since the start of GLP-1RA therapy. Participants also self-reported their daily servings of MyPlate food groups.
Additionally, participants completed a three-day food record using the 2024 version of the Automated Self-Administered Dietary Assessment Tool, which was used to calculate each individual's average intake. The team calculated 95% confidence intervals for each nutrient from the three-day food record relative to their respective daily values based on the DRI.
Findings
In total, 99 individuals were recruited and invited to complete the three-day food record. Of these, only 82 completed a food record, and only 70 completed all three days. The final analytic sample included 69 participants (55 females and 14 males), as one subject with incomplete survey responses was excluded. All participants were currently using a GLP-1RA, with semaglutide and tirzepatide being the most common.
Most participants (39.1%) had been using GLP-1RA for over a year. Notably, 48% of participants planned to take GLP-1RA indefinitely. Further, a majority of the sample (82.6%) was White/Caucasian, and 80% of participants reported that GLP-1RA use resulted in greater weight loss than conventional programs. The most common side effects were nausea, diarrhea, and fatigue.
Approximately one in five subjects (19.3%) reported no side effects. The mean calorie intake was 1,748 kcal/day for the overall sample, 1,700 kcal/day for females, and 1,933 kcal/day for males. This overall average calorie intake, the paper notes, exceeds expert recommendations for individuals on GLP-1RAs (typically 1,200–1,500 kcal/day for females and 1,500–1,800 kcal/day for males). Participants consumed significantly more fat (% of total calories), saturated fat, linoleic acid, alpha-linolenic acid, selenium, sodium, riboflavin, niacin, and vitamin B12 than the DRI.
By contrast, the intake of carbohydrates (both in grams per day and as a percentage of total calories), fiber, calcium, iron, magnesium, potassium, choline, and vitamins A, C, D, E, and K was significantly less than the DRI. Protein intake as a percentage of total calories remained within the Acceptable Macronutrient Distribution Range (AMDR). However, the study highlighted a critical nuance: when assessed on a grams per kilogram of body weight per day (g/kg/day) basis, average protein intake was insufficient to meet the higher needs (1.2–2.0 g/kg/day) recommended during weight loss.
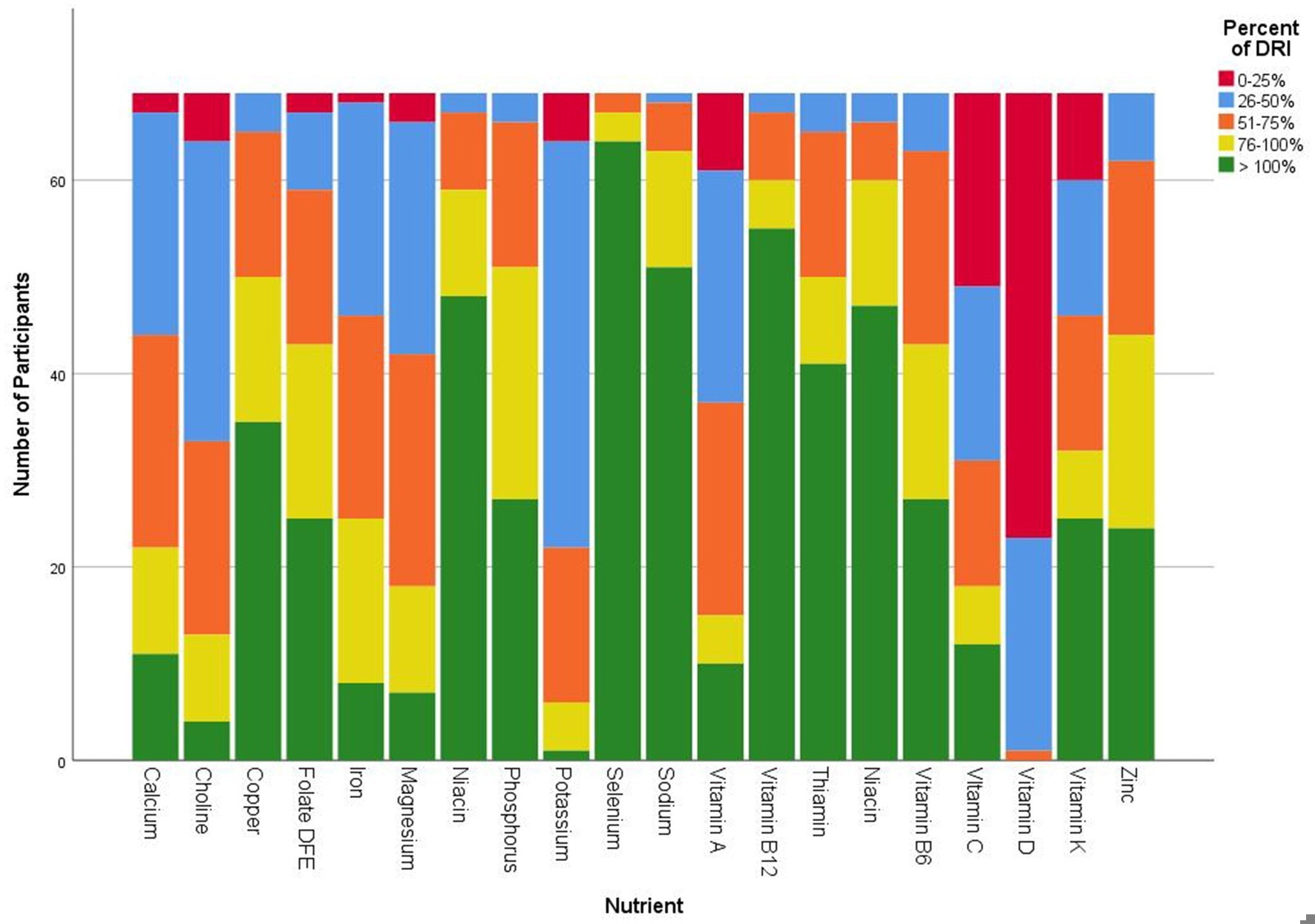 Frequency count categorized three-day average nutrient intake of GLP-1RA participants compared to dietary reference intake.
Frequency count categorized three-day average nutrient intake of GLP-1RA participants compared to dietary reference intake.
This shortfall is particularly concerning because adequate protein is crucial to preserve lean muscle mass during weight loss, a factor critical for long-term metabolic health and weight management; only 43% of participants met the lower end of this g/kg/day recommendation. By intake frequency, vitamin D, potassium, choline, magnesium, and iron had the largest deficits compared to the DRI.
The paper noted that continued poor intake of such essential micronutrients could lead to detrimental long-term health outcomes, including impacts on cardiovascular health and bone density.
There were no significant differences in dietary intake based on participants’ ethnicity, GLP-1RA usage duration, and education. Most participants consumed one to two servings of fruit, grains, dairy, and vegetables and three to four servings of protein per day. Participants under-consumed servings of fruit, grains, dairy, and vegetables compared to MyPlate recommendations.
The study also revealed a potential knowledge gap, as participants often overestimated their fruit and vegetable intake in self-reports compared to their detailed food records, suggesting a need for better dietary education on portion sizes. Furthermore, the paper indicated that standard MyPlate guidance, typically based on a 2,000-calorie diet, may not be tailored for the lower caloric needs or specific nutritional challenges of individuals on GLP-1RA therapy.
Conclusions
Taken together, the overall nutrient intake of participants using a GLP-1RA did not meet MyPlate guidelines or DRI. Participants consumed excess sodium, saturated fat, and calories. Notably, participants consumed inadequate calories from carbohydrates, adequate calories from protein as a percentage of total calories (though critically insufficient in g/kg/day for muscle preservation), and excess calories from fat.
The authors acknowledged certain study limitations and emphasized that these findings underscore the need for patient-centered nutritional guidance, potentially involving Registered Dietitian Nutritionists, to optimize health outcomes and address identified dietary education gaps. Overall, these results may be used for preliminary MNT guidance for this population, and the researchers call for future large-scale studies to confirm these findings and develop more specific nutritional protocols that account for the unique needs of GLP-1RA users.