A new study shows that measuring coronary inflammation with PCAT can spot early heart disease in young adults, even when standard calcium scans show nothing. This breakthrough could change how we identify and treat hidden cardiovascular risk.
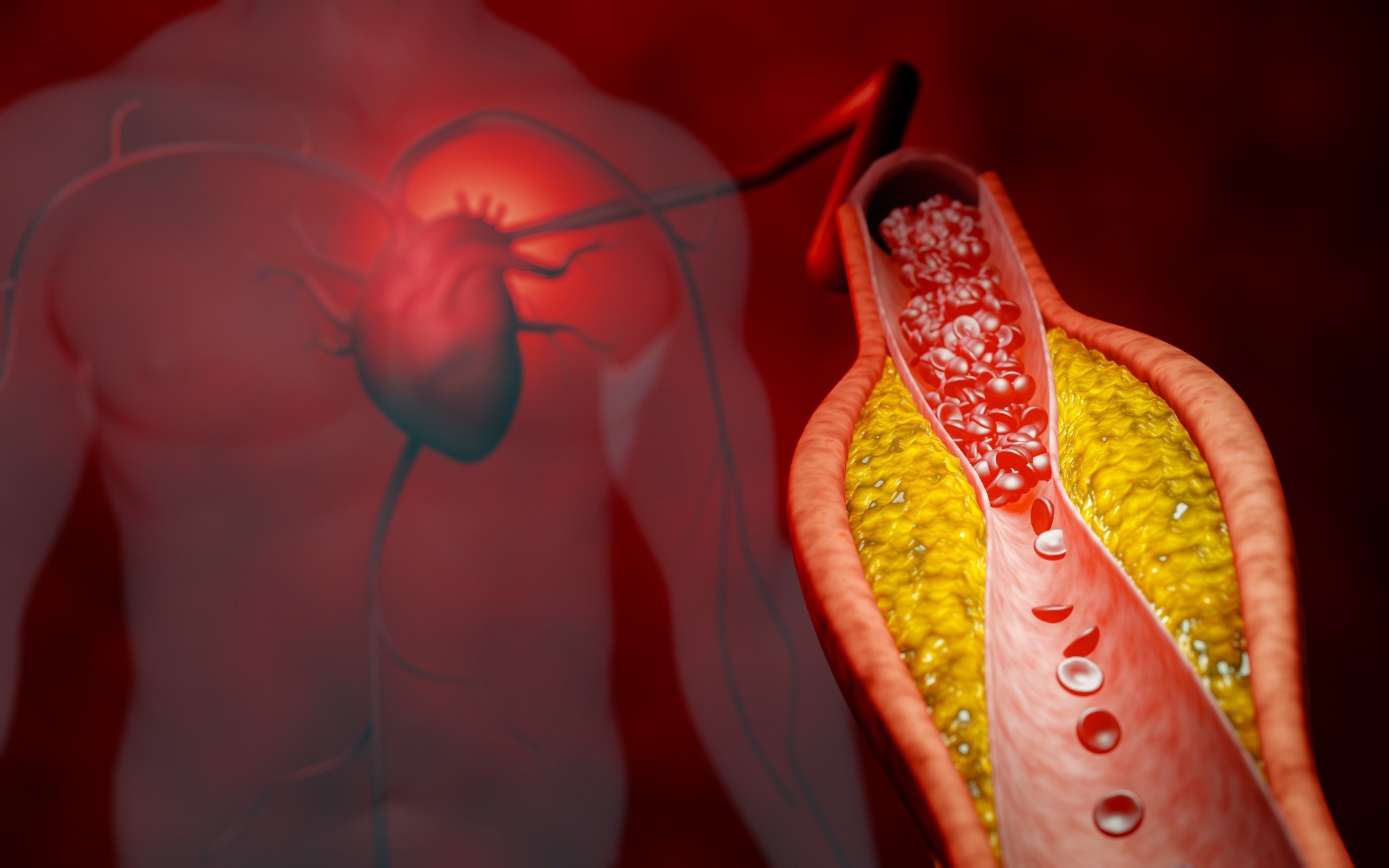 Study: Coronary Inflammation and Atherosclerosis by CCTA in Young Adults (aged 18-45). Image Credit: ridersuperone / Shutterstock
Study: Coronary Inflammation and Atherosclerosis by CCTA in Young Adults (aged 18-45). Image Credit: ridersuperone / Shutterstock
In a recent study published in the American Journal of Preventive Cardiology, researchers investigated the relationship between peri-coronary adipose tissue attenuation (PCAT) and coronary artery disease (CAD) in young people.
Cardiovascular disease (CVD) is the primary cause of death worldwide, with a growing incidence in young adults despite reductions in CVD mortality. Early detection of atherosclerosis in young people is critical, as conventional risk models often underestimate risk in this population. Coronary artery calcium (CAC) scoring and coronary computed tomography angiography (CCTA) are robust tools for detecting early coronary artery disease (CAD).
PCAT is a coronary inflammation marker and plays a crucial role in early atherogenesis. It correlates with the presence and severity of CAD. Identification of premature atherosclerosis by CCTA or CAC scoring can lead to the earlier initiation of prophylactic therapy in individuals who are not otherwise qualified based on traditional risk scoring. As such, PCAT may serve as an adjunctive biomarker to enhance risk stratification.
About the study
In the present study, researchers explored the interplay between PCAT and CAD in a young cohort. Symptomatic adults aged 18–45 who underwent CCTA for suspected CAD between June 2016 and December 2022 were identified from the Montefiore CCTA registry. Clinical and demographic data were obtained from medical records. Cardiac imaging specialists reviewed all CCTA images. CAD was defined as the presence of visible plaque on CCTA or a CAD-Reporting and Data System (CAD-RADS) score ≥ 1.
Obstructive CAD was defined as stenosis ≥ 50% in any coronary artery. The Agatston method was used to estimate the CAC score. Further, a semi-automated software was used for quantitative plaque analysis in segments with a diameter ≥ 2 mm. In subjects with coronary plaque, the volumes of non-calcified plaque (NCP), calcified plaque, total plaque, and low-attenuation plaque were quantified; in patients with CAD, the median total plaque burden was 40.56% and the median total plaque volume was 340.94 mm³.
PCAT was defined as a tissue with -190 Hounsfield units (HU) to -30 HU in a single concentric layer. The average PCAT for each coronary artery was calculated, and the overall PCAT was derived as the average across three coronary vessels: left circumflex (LCX), right (RCA), and left anterior descending (LAD) coronary arteries. Logistic regression models examined the association between CAD and PCAT.
A restricted cubic spline regression analysis was used to assess the relationship between PCAT and CAD risk. A receiver-operating characteristic (ROC) curve analysis evaluated the discriminative ability for CAD using two models; the primary model incorporated established cardiovascular risk factors (hypertension, BMI, smoking, hyperlipidemia, and diabetes), and the other additionally integrated overall PCAT.
Findings
The study included 733 patients, with an average age of 37. Of these, 55% were female and the cohort included diverse ethnicities (44% Hispanic, 23% non-Hispanic Black, 5.3% non-Hispanic White, 3.4% non-Hispanic Asian, and 25.1% Unknown/Others). Around 15% of patients had evidence of CAD on CCTA. CAD patients had a higher prevalence of diabetes, hypertension, hyperlipidemia, family CAD history, and lower levels of high-density lipoprotein cholesterol (HDL-C). Overall, 90.2% of the study population had a CAC score of 0; of these, 34 had evidence of NCP.
Among CAD patients, 13% had obstructive disease, 87% had non-obstructive disease, and 86.8% had mild stenosis. PCAT was -78.94 HU overall, -77.3 HU in the LCX, -80.14 HU in the RCA, and -80.17 HU in the LAD. Males had a higher LCX PCAT than females. CAD patients had a higher overall PCAT, LCX PCAT, and RCA PCAT than non-CAD subjects. Conversely, LAD PCAT was not significantly different between non-CAD and CAD patients.
PCAT was linearly associated with atherosclerosis, as confirmed by a restricted cubic spline regression analysis, with a stronger association observed with increasing PCAT values. PCAT values above specific cutoffs (determined for each coronary artery using the Youden index and termed 'High PCAT' in the study for analytical purposes) were independently associated with CAD, adjusted for sex, age, body mass index (BMI), hypertension, smoking, hyperlipidemia, and family CAD history. In those with a CAC score of 0, CAD patients had significantly elevated LCX PCAT than non-CAD patients.
Besides, there was an association between LCX PCAT and the presence of atherosclerosis, adjusted for hyperlipidemia, family CAD history, and sex. In the ROC curve analysis, the primary model with traditional risk factors achieved moderate discriminative ability for coronary atherosclerosis. However, incorporating overall PCAT in the model, with the paper's discussion highlighting the specific contribution of LCX PCAT, significantly improved the predictive ability.
It is important to note that the authors acknowledged several limitations, including the study's retrospective nature, potential for selection bias as it included only symptomatic patients, the lack of long-term outcome data, and the need for further standardization of PCAT measurement techniques.
Conclusions
In sum, PCAT was elevated in young, symptomatic CAD patients and was associated with the presence of CAD. PCAT was also independently associated with CAD even in patients with a CAC score of 0. Overall, the results emphasize the predictive value of PCAT in a young population, suggesting its role as a novel non-invasive marker for detecting CAD. Incorporating PCAT into clinical practice could improve risk stratification and identify those who may benefit from early intervention.