A decade-long Canadian study reveals that the timing of natural menopause does not affect the risk of hypothyroidism, but women with higher BMI face greater odds.
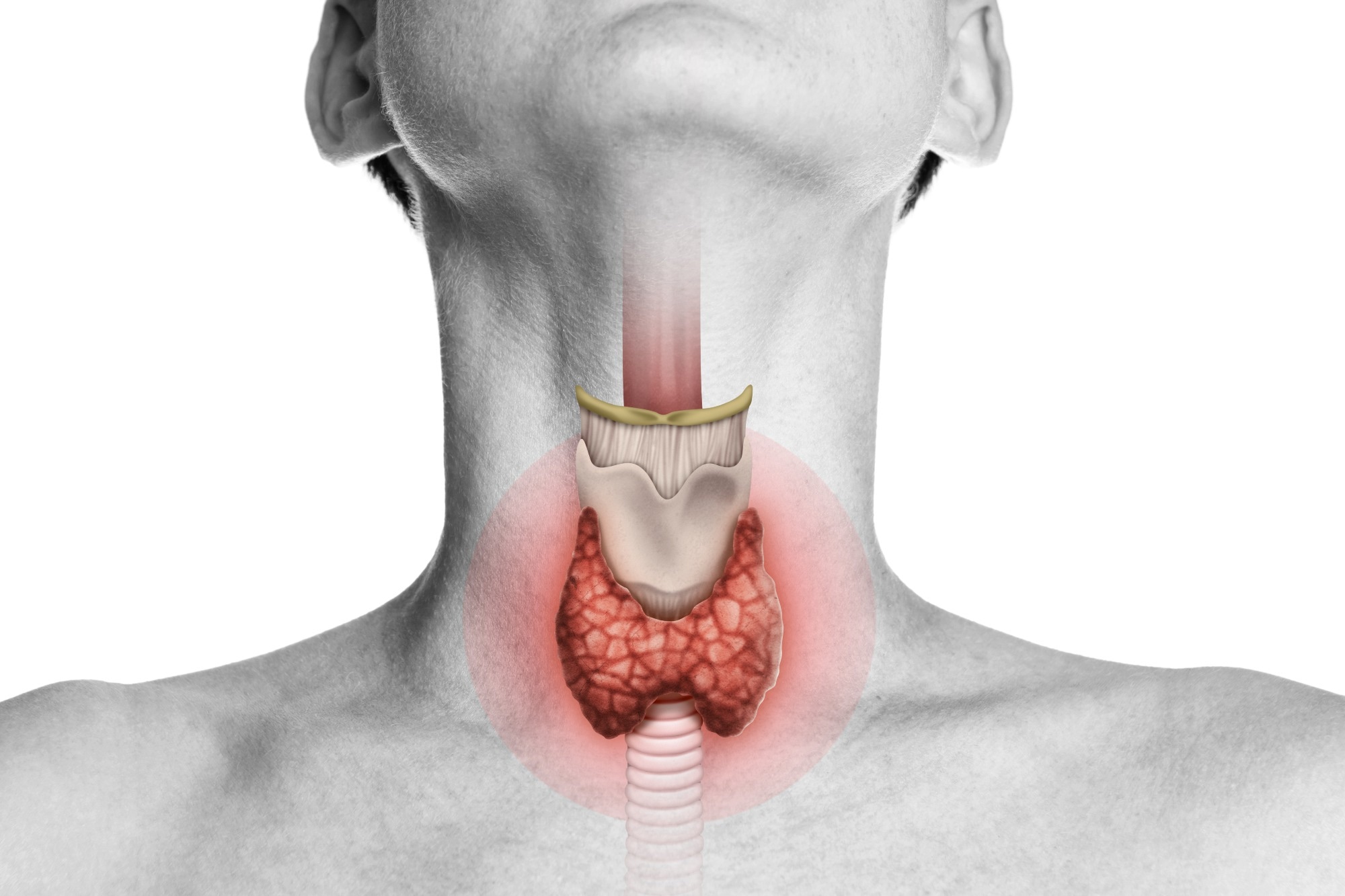 Study: Associations between age at natural menopause and risk of hypothyroidism among postmenopausal women from the Canadian Longitudinal Study on Aging (CLSA). Image Credit: SvetaZi / Shutterstock
Study: Associations between age at natural menopause and risk of hypothyroidism among postmenopausal women from the Canadian Longitudinal Study on Aging (CLSA). Image Credit: SvetaZi / Shutterstock
In a recent article published in the journal PLOS One, researchers investigated the association between age at natural menopause (ANM) and the risk of developing overt hypothyroidism among postmenopausal Canadian women.
After following women for 10 years, they found no significant association between ANM and the incidence of hypothyroidism.
Background
Hypothyroidism occurs when the thyroid gland underproduces hormones that regulate organ function, metabolism, and temperature. Its symptoms include goiter, depression, fatigue, and weight gain. In developed countries, autoimmune causes are the leading contributor to hypothyroidism, which disproportionately affects women, especially with increasing age.
The hormonal interplay between thyroid function and menopause, with both influencing reproductive hormones, has raised interest in how reproductive milestones might impact thyroid health. Menopause, which typically occurs around age 51, leads to a sharp decline in estrogen, which may affect the metabolism of the thyroid hormone.
Notably, 70% of hypothyroidism cases are diagnosed in women over 50, and subclinical hypothyroidism is common during menopausal transition. Early menopause has been linked to an increased risk of autoimmune conditions and thyroid dysfunction. For example, 20–35% of women with premature ovarian failure also have thyroid autoimmunity.
Although some reproductive factors, such as the use of oral contraceptives, menarche, and pregnancy, have been studied to examine how they influence hypothyroidism risk, findings are inconsistent. For example, hypothyroidism shows significant decreases during pregnancy, but sharp increases after childbirth, and associations with the use of oral contraceptives are mixed.
However, this is the first large-scale longitudinal study to examine ANM and overt hypothyroidism (clinically diagnosed), addressing a gap in prior research that focused only on subclinical forms with conflicting outcomes. This could lead to improved guidelines to manage hypothyroidism risk for older women.
About the Study
Given estrogen's potential role in thyroid regulation, this study aimed to explore whether ANM is associated with the incidence of hypothyroidism in postmenopausal women, using data from the Canadian Longitudinal Study on Aging (CLSA), which collected data across three cycles over a 10-year period, employing a retrospective cohort design.
Researchers excluded participants who had not reached menopause, had surgical or medical menopause, had missing menopause age or relevant hypothyroidism data, were diagnosed with hypothyroidism before menopause, or had ANM <40 or >67 years (aligning with Verschoor & Tamim cutoffs).
Incident hypothyroidism was assessed through self-reported diagnosis and age at diagnosis. The primary outcome was the time to onset of hypothyroidism after menopause. Participants not developing hypothyroidism contributed censored data.
Covariates included sociodemographic characteristics (ethnicity, education), health behaviors (smoking, alcohol use, physical activity), body mass index (BMI), and reproductive history (age at menarche, use of oral contraceptives and hormone therapy, number of births). Data on these covariates were collected from different CLSA cycles and utilized multiple imputation to address missingness in key variables (e.g., oral contraceptive duration).
Statistical analysis involved survival models, with Cox proportional hazards regression used to estimate associations between ANM and hypothyroidism. Models were adjusted for all relevant covariates and tested interactions between ANM and BMI/HRT (none were significant). Robust standard errors addressed proportional hazards assumption violations detected via log-log plots.
Findings
This study analyzed data from 15,330 postmenopausal women over 257,589.7 person-years to assess the association between ANM and the incidence of hypothyroidism. A total of 1,674 women (10.9%) reported hypothyroidism, yielding an incidence rate of 6.5 per 1,000 person-years.
The average baseline age was 60.6 years, and the median age at menopause (ANM) was 50 years. Most participants were White (94.4%) and aged 45–64 (68.5%) at baseline. Approximately 71.1% never used hormone replacement therapy, 52.8% engaged in regular physical activity, and 36.8% had a normal body mass index (BMI).
Survival curves showed no significant difference in the onset of hypothyroidism across ANM groups (log-rank p = 0.7). Multivariable Cox regression analysis also showed no statistically significant association between ANM and hypothyroidism risk.
However, BMI was significantly linked with hypothyroidism: women with a BMI of 25–29 had a 20% increased risk (HR 1.2), and those with a BMI of ≥30 had a 40% increased risk (HR 1.4). The authors note that hypothyroidism may contribute to weight gain (through reduced metabolic rate), suggesting BMI could be a consequence of thyroid dysfunction rather than solely a risk factor.
Conclusions
This large-scale longitudinal study found no link between ANM and overt hypothyroidism incidence. This aligns with one prior subclinical hypothyroidism study but contrasts with others, possibly due to differences in study populations (e.g., inclusion of surgical menopause) or diagnostic criteria.
Higher BMI was consistently associated with increased hypothyroidism risk, though the directionality remains unclear (obesity may be a consequence of thyroid dysfunction). Estrogen’s role in increasing thyroid-binding globulin (TBG) without affecting free T4 in healthy women may explain why ANM showed no association.
The strengths of this study include the large, population-weighted sample and detailed sociodemographic and health data. However, limitations include self-reported diagnoses and BMI, potential misclassification, and underdiagnosis due to symptom overlap with aging. The lack of direct hormone measurements may have reduced diagnostic accuracy. Generalizability is somewhat limited due to cohort-specific exclusions and because most participants were White.
In conclusion, ANM was not associated with hypothyroidism risk, but higher BMI was. Future research should include hormone assays, longitudinal analysis of BMI-thyroid relationships, and explore estrogen’s specific effects on thyroid metabolism.