New genetic evidence challenges common beliefs about vitamin supplements for diabetes, revealing that too much vitamin B6 may increase the risk of dangerous low blood sugar episodes.
 Image Credit: Suriyawut Suriya / Shutterstock
Image Credit: Suriyawut Suriya / Shutterstock
In a recent study published in the journal Food Science & Nutrition, researchers utilized several large-scale genome-wide association study (GWAS) datasets, along with cutting-edge Mendelian Randomization (MR) statistical models, to elucidate the causal associations between circulating vitamin concentrations and diabetic complications in patients with diabetes.
Their study focused on vitamins A, B6, C, and D, represented by participant groups of 5,006, 64,974, 52,018, and 441,291 individuals, respectively. From these groups, the study used 2, 1, 10, and 166 genetic variants (SNPs) for each vitamin, respectively.
Study findings suggest that vitamins are not the silver bullets against diabetes that health professionals previously thought they were. Vitamins A, C, and D did not demonstrate any statistical association with diabetes complications, contradicting previous reports of their beneficial effects.
Furthermore, Vitamin B6 concentrations were strongly associated with diabetic hypoglycemia (odds ratio [OR] = 8.54; p = 0.0075), identifying the vitamin as a potential risk factor in disease progression and highlighting the potential need for vitamin monitoring and accurate supplement advice; however, the authors urge caution in interpreting this specific result.
Background
Diabetes mellitus (DM), often referred to as 'diabetes', is an umbrella term for a group of chronic metabolic diseases characterized by the body's inability to sufficiently regulate its insulin secretion, resulting in elevated blood sugar (glucose) levels. DM represents a persistent and pressing global public health crisis, particularly in today's fast-paced society, plagued by suboptimal health behaviors (sleep, diet, physical activity).
The International Diabetes Federation (IDF) estimates that DM (alongside its comorbidities) contributes to ~6.7 million human deaths annually, highlighting the need for intensive research aimed at identifying DM's risk factors and therapeutic interventions. Given their extensive importance in human growth, development, homeostasis, and metabolism, vitamins (Vits) have long been studied for their potential in mitigating DM outcomes.
Vitamins D, C, A, and B6 are of special interest given their proven metabolic and anti-inflammatory properties. However, the literature is conflicting, with some studies suggesting that vitamin supplementation alleviates DM symptoms, while others claim that higher vitamin concentrations exacerbate the condition. While recent research has validated the strong correlation between DM and chronic inflammation, causal associations between vitamin concentrations and DM remain lacking.
About the study
The present study aims to address this knowledge gap and inform diabetic patients and clinicians alike by collating several publicly available genome-wide association study (GWAS) datasets and leveraging a relatively novel statistical method termed 'Mendelian Randomization (MR)' to elucidate causal associations between genetic (GWAS-derived) data, circulating vitamin concentrations, and DM complications.
Methodological design and outcomes reporting adhered to the Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization (STROBE-MR) guidelines. Study data were obtained from the European Prospective Investigation into Cancer and Nutrition (EPIC) cohorts, the University of Bristol's MRC Integrative Epidemiology Unit (IEU) consortium, and the FinnGen GWAS datasets. Participant inclusion was restricted to individuals of European descent to prevent genetic biases.
Single-nucleotide polymorphisms (SNPs; p < 5×10⁻⁸) were extracted for use as genetic instruments and were subjected to rigorous pruning, linkage disequilibrium (r²<0.001), and QC to ensure data robustness. Exposure factors of interest, including the circulating concentration of Vits A, B6, C, and D, were analyzed against outcome data for six diabetic complications from the FinnGen consortium, which includes up to 500,000 participants. The strength of the statistical association between exposures and their corresponding SNPs was evaluated to ensure instrument validity.
Finally, statistical analyses employed several inverse-variance weighted (IVW), MR (MR-Egger, weighted median, MR-PRESSO), and leave-one-out models, all of which were corrected for demographic variables. Cochran's Q and MR-Egger were used to establish the reliability of outcomes via Heterogeneity and pleiotropy checks, respectively.
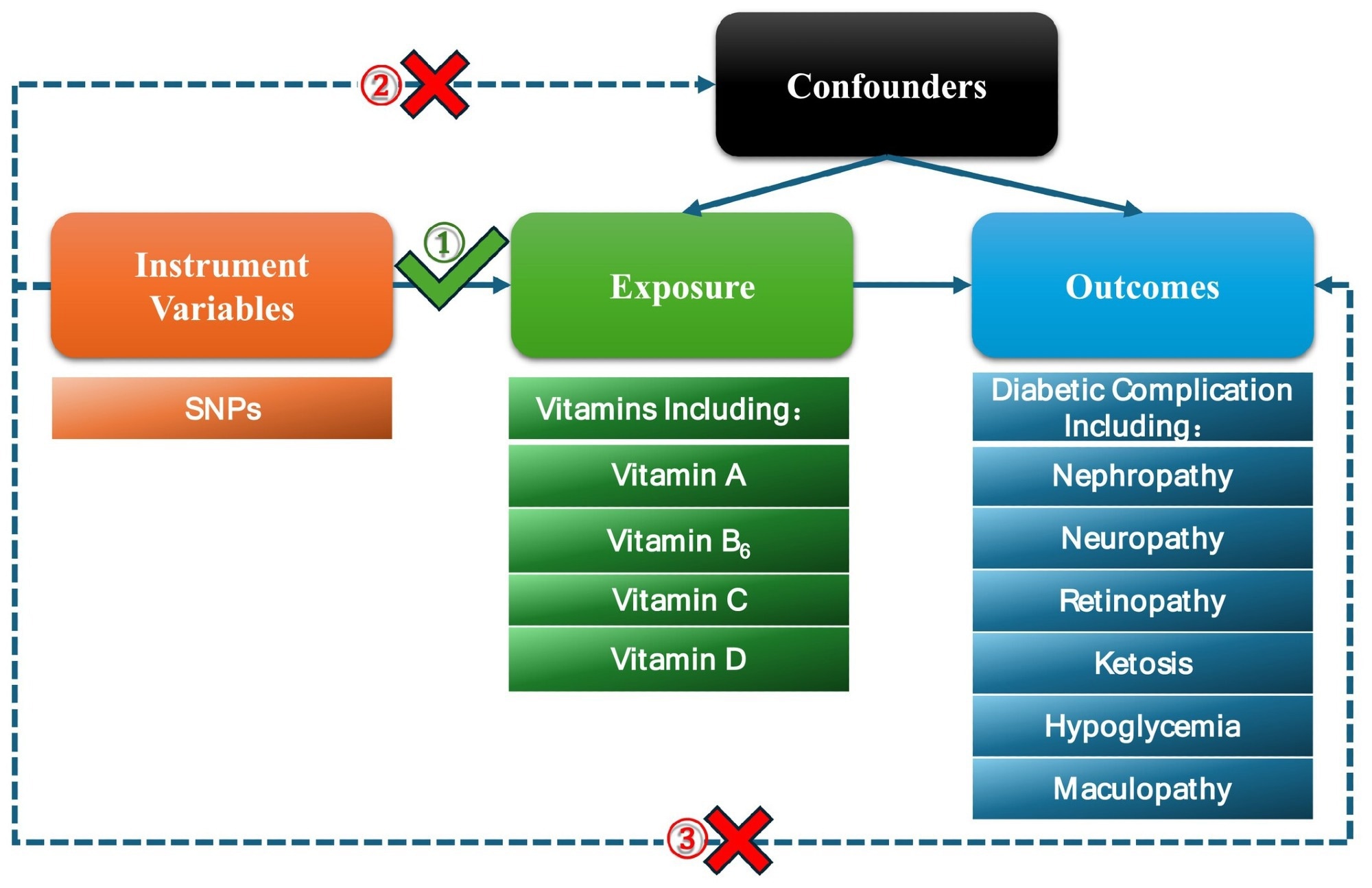 Flow chart of the Mendelian randomization (MR) study and three key assumptions. Firstly, the selected single nucleotide polymorphisms (SNPs) are strongly associated with exposure; vitamins are used as exposure factors in this article. Secondly, there is no association between the SNPs and confounders. Finally, the SNPs can only impact outcomes (diabetic complications) through vitamins directly.
Flow chart of the Mendelian randomization (MR) study and three key assumptions. Firstly, the selected single nucleotide polymorphisms (SNPs) are strongly associated with exposure; vitamins are used as exposure factors in this article. Secondly, there is no association between the SNPs and confounders. Finally, the SNPs can only impact outcomes (diabetic complications) through vitamins directly.
Study findings
Contrasting previous reports and widely-held beliefs, the present study was unable to establish an association between higher Vit concentrations and subsequent DM benefits. VitA concentrations failed to demonstrate any link with any DM subgroup under consideration (maculopathy, ketoacidosis, nephropathy, neuropathy, or retinopathy). Its odds ratios (ORs) were observed to range from 0.95 (hypoglycemia) to 2.62 (maculopathy), but p-values never reached significance.
VitC mirrored VitA results, demonstrating no causal association with any DM subtype. While VitD initially appeared protective against ketoacidosis (OR 0.74, p=0.04), this link vanished after MR-PRESSO outlier correction (OR 0.76, p=0.055). No associations were detected for other complications (e.g., hypoglycemia, OR 0.86, p = 0.37).
In contrast, Vitamin B6 showed a striking result: a genetically predicted elevation was associated with a dramatic 8.54-fold increase in diabetic hypoglycemia risk (95% CI: 1.77-41.2; p = 0.0075). However, the authors stress that this finding must be treated with significant caution.
The result is based on a single genetic variant, and the very wide confidence interval (1.77 to 41.2) suggests the potential for overestimation. The paper discusses this as a potential "paradox," where Vitamin B6's known ability to lower blood glucose might, in excess, lead to dangerously low levels (hypoglycemia).
Conclusions
The present study addresses the vitamin-use-in-diabetes debate by contradicting the popular view of vitamins’ beneficial DM outcomes. It provides preliminary genetic evidence that elevated Vitamin B6 levels may causally increase the risk of diabetic hypoglycemia, though this requires significant further confirmation. Vitamins A, C, and D showed no causal relationship with complications such as nephropathy, retinopathy, ketoacidosis, or maculopathy in the studied European population.
Further research is needed to uncover mechanisms, confirm these findings in more robust and diverse populations, and determine safe intake thresholds. Clinicians and patients should focus on personalized vitamin strategies, balancing the risks of deficiency with potential harm, because, as this study suggests, in diabetes, too much of what we believe to be beneficial may sometimes be dangerous.
Journal reference:
- Cai, S., Man, W., Liu, W., Li, B., He, Z., & Duan, G. (2025). Causal Relationship Between Various Vitamins and Different Diabetic Complications: A Mendelian Randomization Study. Food Science & Nutrition, 13(7). DOI:10.1002/fsn3.70536. https://onlinelibrary.wiley.com/doi/10.1002/fsn3.70536.