By embedding autonomous AI screening directly into safety-net primary care, researchers hope to speed up diabetic retinopathy diagnosis, strengthen referral follow-through, and help millions at risk of vision loss receive timely treatment.
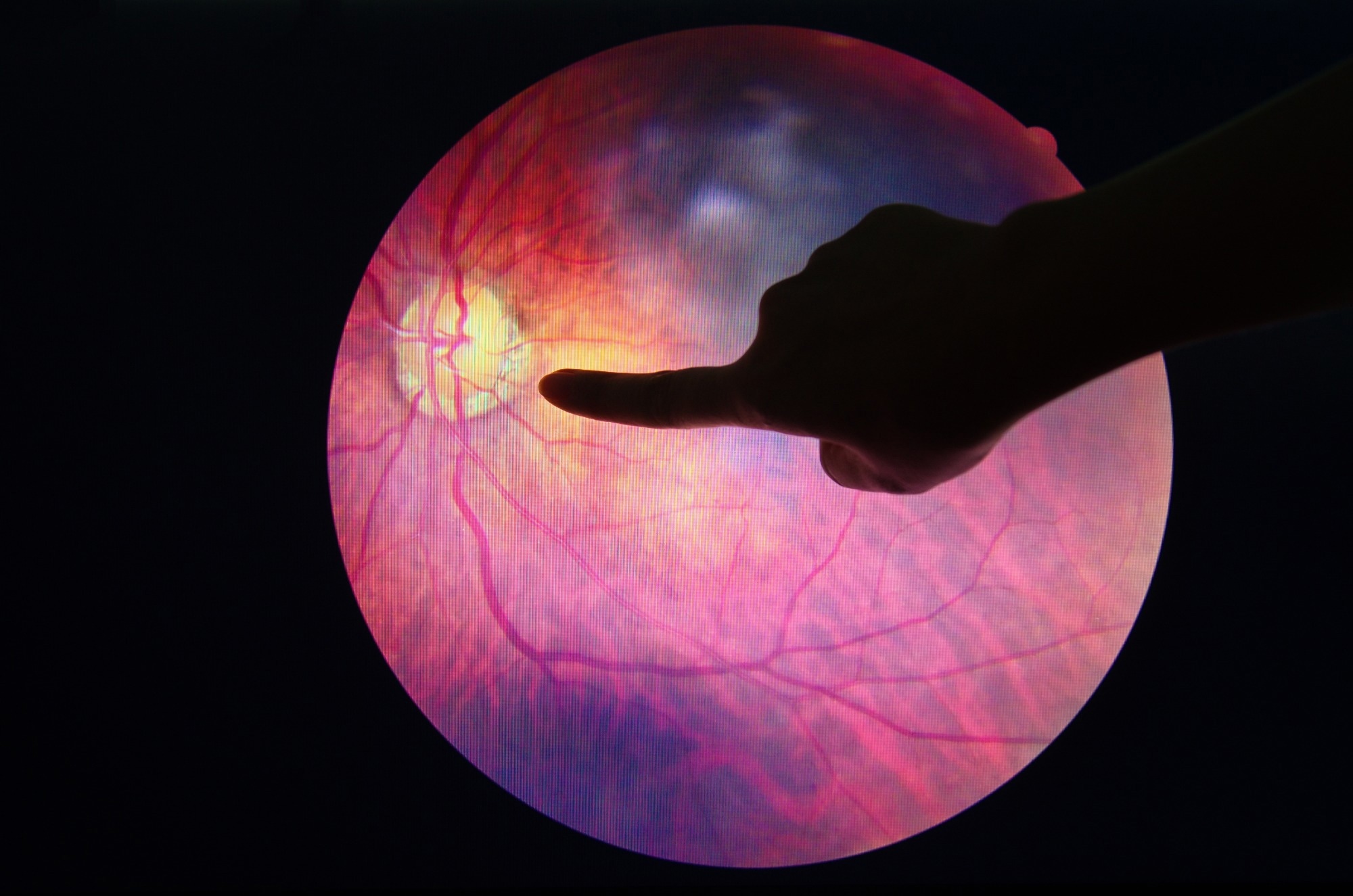
Trial: Diabetic Retinopathy Screening Among Federally Qualified Health Center Patients Using Point-of-Care AI. Image Credit: Anukool Manoton / Shutterstock
In a recent trial protocol published in the JAMA Network Open, a group of researchers will test whether point-of-care autonomous AI screening embedded in federally qualified health center (FQHC) workflows improves diabetic retinopathy (DR) screening completion, speeds diagnosis, and strengthens referral follow-through and patient experience.
Background
One in four people with diabetes in the U.S. shows early signs of DR, yet symptoms are often invisible until vision is threatened. Annual eye checks prevent avoidable blindness, but many patients miss referrals because of time, travel, and cost barriers. FQHCs serve 32.5 million people who face these hurdles. Autonomous AI that reads fundus photos during a routine visit can return a result on the spot, turning a missed referral into same-day action. However, equity, workflow fit, and patient trust remain open questions, for which further research is urgently needed.
About the study
This randomized, open-label, patient-level, parallel-group trial enrolls adults with diabetes who have not completed DR screening within 11 months at two FQHC clinics at San Ysidro Health in San Diego County, California. Recruitment began in June 2024 and is anticipated to conclude in August 2025, with follow-up through February 2026. Participants provide consent, complete baseline surveys, and are randomized to point-of-care screening with an autonomous artificial intelligence diabetic retinopathy system (AI-DRS) or to usual-care referral. In the intervention arm, nonmydriatic fundus photographs are acquired on a Topcon TRC-NW400 camera by trained staff after a two-day competency program. Images are analyzed by an algorithm cleared by the FDA (EyeArt; Eyenuk Inc). The algorithm classifies more-than-mild diabetic retinopathy (mtmDR) and vision-threatening diabetic retinopathy (VTDR); three failed quality attempts yield an ungradable result.
Results flow into the electronic health record (EHR) via HL7 integration, triggering risk-stratified referrals for primary care practitioner (PCP) review, immediate retina referral for positives, and urgent ophthalmology referral for ungradable images. Both study arms receive standard referrals and participant navigation support for appointment booking. Outcomes at 90 and 180 days include screening completion (primary), stage at first detection, referral completion, and patient-reported knowledge, attitudes, self-efficacy, and satisfaction. The protocol follows Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) and is guided by the Pragmatic Robust Implementation and Sustainability Model (PRISM).
Study results
This protocol prespecifies outcomes and the analytic plan. The primary endpoint is the completion of DR screening within 90 days, a patient-centered measure linked to earlier diagnosis and treatment. Secondary endpoints include DR stage at first detection, completion of risk-stratified referrals, and changes in knowledge, attitudes, and self-efficacy toward point-of-care AI. EHR integration enables tracking of orders, show rates, and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes after eye-care visits. Implementation metrics such as successful image acquisition, ungradable rates after three attempts, and camera time per patient quantify feasibility in busy clinics. Patient-reported measures adapted from validated instruments assess trust and comfort with autonomous AI as routine care.
Evidence motivating the intervention comes from prior evaluations of the same FDA-cleared AI-DRS. Against the Early Treatment Diabetic Retinopathy Study (ETDRS) reference standard, the sensitivity for mtmDR was 96% (specificity, 88%), and the sensitivity for VTDR was 97% (specificity, 90%), with conclusive outputs for more than 97% of eyes, typically without dilation. In more than 100,000 real-world encounters, sensitivity and specificity were both about 91% for mtmDR detection. These performance characteristics suggest that on-site screening can accurately triage patients and reduce missed referrals.
Workflow integration is central to impact. Orders originate in the EHR and route to the AI-DRS server; the desktop client guides acquisition with real-time quality feedback. After analysis, results return to the EHR to prompt PCP review and risk-based referrals. Patients positive for VTDR or mtmDR receive immediate retina appointments (target ≤ 24 hours). Patients with ungradable images, often a marker of underlying pathology, receive urgent ophthalmology appointments (target ≤ 72 hours). Patients negative for both mtmDR and VTDR are scheduled for repeat screening in 12 months. This closed-loop design is intended to shrink diagnostic delays and increase adherence.
To support reporting, DR findings are mapped to ICD-10 codes, covering both nonproliferative and proliferative stages, with and without macular edema. This enables consistent documentation, audit, and population-health dashboards within FQHC systems. Analyses will use regression models with covariate adjustment for clinic site, demographics, and clinical risk, with difference-in-differences for survey changes. Implementation will be evaluated through PRISM domains (reach, adoption, implementation, and maintenance) to understand what it takes to sustain AI-enabled screening in safety-net settings. If the AI-DRS achieves or exceeds screening benchmarks, the model could help clinics reach performance targets such as the 63% “high-performance level” as specified in the protocol’s PRISM outcomes.
Finally, the protocol includes oversight and safety monitoring. Although no formal safety endpoints are planned, adverse events will be recorded and reviewed by a Data Safety Monitoring Committee. Algorithms remain static during the trial to avoid performance drift, and staff training emphasizes competency checks and troubleshooting for reliable image capture. Generalizability may be constrained by reliance on Epic EHR integration, equipment and licensing costs, and trained personnel requirements.
Conclusions
This pragmatic protocol evaluates whether embedding autonomous AI-DRS within FQHC primary care, backed by FDA clearance, ETDRS-referenced accuracy, and HL7-enabled EHR interoperability, can lift DR screening completion, accelerate diagnosis, and strengthen referral adherence. By returning results in minutes and mapping findings to ICD-10 for consistent reporting, the model aims to reduce avoidable vision loss while simplifying workflows for PCPs. Guided by SPIRIT for transparent reporting and PRISM for real-world implementation, the approach offers a practical roadmap, such as training, closed-loop referrals, and quality monitoring, that safety-net clinics can adapt to improve population eye health at scale.
Trial registration: NCT06721351. Two coauthors are employees of Eyenuk Inc. and report related patents; other authors report no relevant disclosures.
Journal reference:
- Diaz, E. A., Seifert, M. L., Gruning, V., Stadnick, N. A., Lugo-Butler, E., Servin, A. N., Rodríguez-Rosales, C. I., Geremia, C., Ramachandra, C., Bhaskaranand, M., Howard, D., Solis, O., Velasquez, S., Snook, B., Tucker, S., & Muñoz, F. A. (2025). Diabetic Retinopathy Screening Among Federally Qualified Health Center Patients Using Point-of-Care AI: DRES-POCAI: A Trial Protocol. JAMA Network Open, 8(10). DOI: 10.1001/jamanetworkopen.2025.38114 https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2840380