New evidence shows that GLP-1–based therapies not only lower glucose levels and aid in weight loss but also reduce inflammation in the heart, kidneys, liver, and brain, revealing a broader therapeutic potential beyond metabolism.
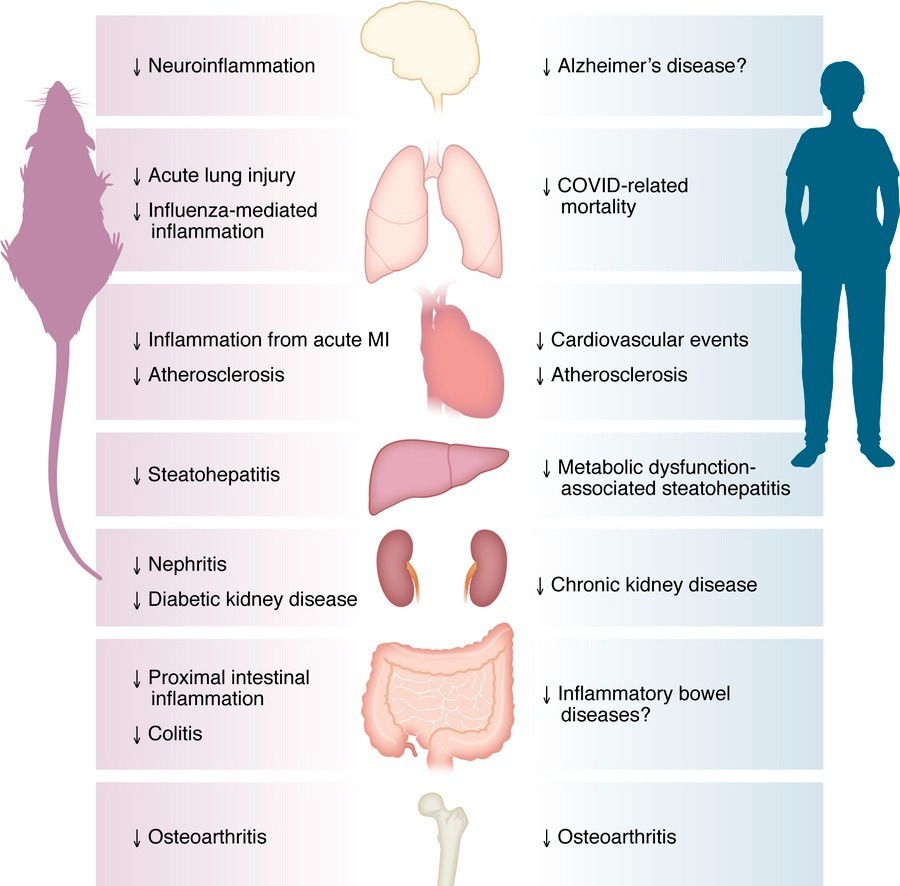
Antiinflammatory actions of GLP-1 medicines across organs. GLP-1R agonists exert broad antiinflammatory effects in multiple peripheral organs, including the central nervous system, lungs, cardiovascular system, liver, intestine, kidneys, and joints. Evidence from both preclinical and clinical studies supports their antiinflammatory roles in the cardiovascular system, liver, kidneys, and joints. However, the potential antiinflammatory effects of GLP-1 signaling in the central nervous system, lungs, and intestine remain to be fully elucidated and warrant further investigation.
In a recent study published in the Journal of Clinical Investigation, researchers reviewed the anti-inflammatory effects and mechanisms of glucagon-like peptide 1 (GLP-1)-based therapies.
The development of GLP-1 medicines has transformed the therapeutic options for patients with type 2 diabetes (T2D) who are unable to achieve sufficient glucose control with existing treatments. These medicines have also yielded meaningful benefits for obese individuals who were unable to achieve adequate weight reduction through lifestyle modifications. GLP-1 medicines decrease the rates of complications associated with obesity and T2D.
A growing body of evidence suggests that GLP-1 has anti-inflammatory actions independent of its metabolic actions. Understanding how GLP-1 regulates inflammation will provide insights into the pleiotropic benefits of GLP-1 receptor (GLP-1R) agonism. In the present study, researchers summarized the anti-inflammatory effects of GLP-1 medicines, covering emerging concepts and their clinical relevance.
Anti-inflammatory effects of GLP-1 medicines independent of weight loss
Several GLP-1 medicines, including semaglutide, liraglutide, and exenatide, reduce plasma levels of C-reactive protein (CRP), a surrogate of systemic inflammation, in people with obesity or T2D. This may be partly mediated by improvements in weight loss and glucose control. In the large SUSTAIN and PIONEER trials, only about 20–60% of the CRP reduction was explained by weight and glycaemia. In PIONEER-2, oral semaglutide reduced CRP, whereas empagliflozin did not, despite similar weight loss. More potent medicines, such as semaglutide, tirzepatide, and liraglutide, may have superior anti-inflammatory effects.
Nonetheless, GLP-1 medicines also exert anti-inflammatory effects independent of their metabolic effects. For instance, a single dose of semaglutide or exenatide reduced circulating levels of tumor necrosis factor (TNF-α) in mice challenged with lipopolysaccharide (LPS). Moreover, exenatide downregulates TNF and interleukin-1β (IL1B) in human peripheral blood mononuclear cells. These effects manifest within hours, preceding any meaningful weight reduction. Additionally, IL-6 infusion elevates GLP-1 in mice but not in humans, underscoring species-specific regulation of inflammation.
GLP-1 medicines in neuro- and cardiovascular inflammation
Microglia secrete pro-inflammatory cytokines upon activation, stimulating nearby reactive astrocytes and amplifying local neuroinflammation. A five-month treatment with PEGylated exenatide (NLY01) was found to decrease the secretion of complement 1q (C1q), IL-1α, and TNF-α by primary mouse microglia, thereby limiting the conversion of astrocytes to a neurotoxic phenotype. It is unclear whether these neural anti-inflammatory actions of GLP-1 medicines rely on GLP-1R activity. Many neuroprotective effects remain to be causally associated with anti-inflammatory mechanisms, and some Alzheimer’s disease mouse models did not respond to semaglutide or tirzepatide, emphasizing that not all neural benefits are consistent across studies.
In mouse models of Parkinson's disease, treatment with NLY01 for five months was protective against neurodegeneration. Furthermore, in a transgenic mouse model of Alzheimer’s disease, treatment with liraglutide was associated with improvements in memory function. However, the review stresses that direct attribution of these effects to GLP-1R-mediated anti-inflammatory pathways remains to be conclusively demonstrated.
A 14-week treatment with liraglutide was reported to decrease the size of atherosclerotic plaques in the aortas of mice. In contrast, control mice with matching weight loss were not protected from atherosclerosis, suggesting that liraglutide has anti-atherogenic effects independent of weight loss. Similarly, semaglutide reduces plaque size and burden, as well as downregulates a pro-inflammatory gene program, in mice.
In mice with acute myocardial infarction, liraglutide treatment decreased atrial IL6 expression and circulating IL-6 levels. Further, clinical trials show that long-acting GLP-1 medicines decrease cardiovascular events in individuals with T2D or obesity. These benefits occur quickly following treatment initiation, suggesting that GLP-1 medicines may reduce cardiovascular events, at least in part, through weight loss-independent mechanisms. The review also notes that GLP-1 medicines reduce complications in conditions such as obstructive sleep apnea (OSA), expanding their cardiometabolic relevance.
GLP-1 medicines in kidney and liver inflammation
Treatment with an exenatide analog was found to significantly decrease hepatic lipid accumulation, liver weight, and plasma levels of alanine transaminase in mice on a high-trans-fat diet; these effects were abrogated in Glp1r-null mice on the same diet. Clinical trials have reported favorable outcomes with GLP-1 medicines in individuals with metabolic dysfunction-associated steatohepatitis.
In a clinical trial, one-year dulaglutide treatment in individuals with chronic kidney disease (CKD) and T2D resulted in an increased estimated glomerular filtration rate compared to insulin glargine. In a separate trial involving T2D patients, semaglutide treatment decreased the risk of CKD and cardiovascular death by 24%, delaying the progression of kidney dysfunction over four years. The review also emphasized that the renal and hepatic benefits of GLP-1 medicines appear mechanistically linked to both systemic metabolic improvements and local anti-inflammatory signaling.
GLP-1 medicines in arthritis and pulmonary inflammation
A single dose of liraglutide administered before LPS exposure in mice was found to attenuate lung injury, reducing the expression of IL-6, IL-1β, and TNF in the lungs. Likewise, daily liraglutide treatment downregulated lung C-C motif chemokine ligand 2 (Ccl2) and IL-6 in mice during influenza infection. Similarly, a single dose of semaglutide downregulated lung IL-1β, TNF, and IL-6 expression in a polymicrobial sepsis-induced lung inflammation model. Findings in the lung are model-dependent; liraglutide exacerbated bleomycin-induced lung injury in mice, contrasting with protective effects in LPS, influenza, and sepsis models.
In an osteoarthritis model, a single liraglutide injection decreased synovitis and pain sensitivity, without affecting body weight. In mouse primary chondrocytes stimulated with IL-1β, liraglutide treatment downregulated Tnf and nitric oxide synthase 2 (Nos2). In a clinical trial involving obese individuals with knee osteoarthritis, semaglutide was associated with a greater improvement in an osteoarthritis index score. However, the review notes that these results, while promising, remain preliminary and require confirmation in larger outcome studies.
Mechanistic and receptor expression considerations
The review highlights that GLP-1R expression in peripheral immune and non-immune tissues is very low and technically challenging to detect, necessitating the use of validated multimodal methods. Anti-inflammatory actions likely arise through both direct GLP-1R activation in rare cell types and indirect neural or metabolic crosstalk. Tirzepatide’s dual GLP-1R and GIPR agonism may confer distinct anti-inflammatory effects, some of which persist even when neuronal GLP-1R signaling is impaired.
Concluding remarks
Although peripheral organs have relatively low GLP-1R expression, GLP-1 medicines exert anti-inflammatory effects through indirect and direct mechanisms involving neural, immune, and vascular crosstalk. Given these anti-inflammatory effects, there is speculation that GLP-1 medicines could impair host immune defenses; however, current evidence does not indicate a higher risk of infection or obesity-related cancer. Although cholecystitis has been reported, large outcome trials have not substantiated pancreatitis signals, and current evidence does not indicate increased risks of infection or obesity-related cancers. The review further distinguishes between established outcome benefits (CVD, CKD, and OSA) and conditions still under investigation (neurodegeneration, arthritis, and some liver endpoints).
Journal reference:
- Wong CK, Drucker DJ (2025). Antiinflammatory actions of glucagon-like peptide-1–based therapies beyond metabolic benefits. The Journal of Clinical Investigation, 135(21), e194751. DOI: 10.1172/JCI194751. https://www.jci.org/articles/view/194751