New research shows that certain flavonols from everyday foods can shut down the body’s drug-resistance machinery, potentially paving the way for more effective treatments, but clinical hurdles remain.
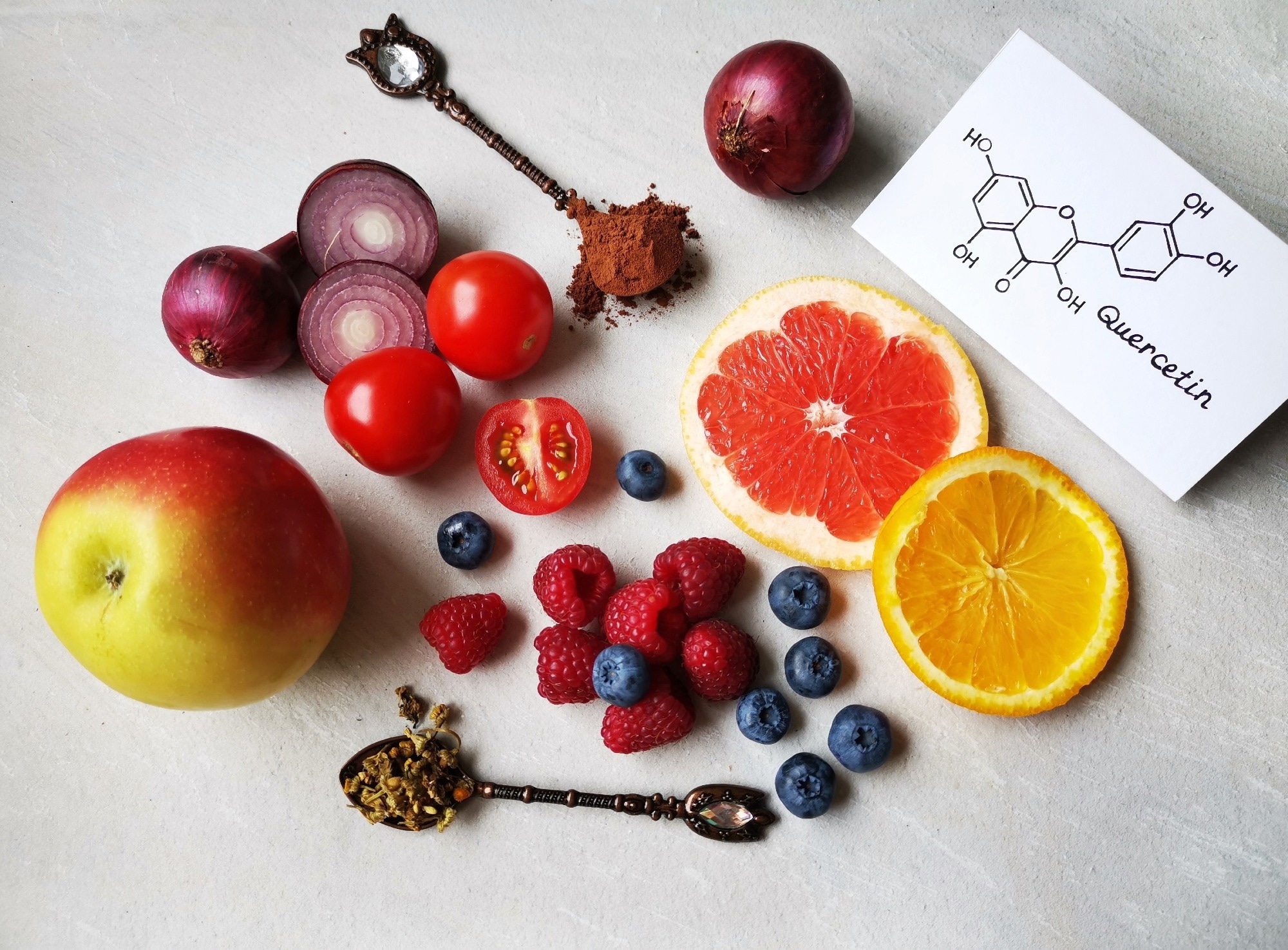 Study: Inhibition of breast cancer resistance protein by flavonols: in vitro, in vivo, and in silico implications of the interactions. Image Credit: Danijela Maksimovic / Shutterstock
Study: Inhibition of breast cancer resistance protein by flavonols: in vitro, in vivo, and in silico implications of the interactions. Image Credit: Danijela Maksimovic / Shutterstock
In a recent study published in the journal Scientific Reports, a group of researchers identified flavonols that inhibit Breast Cancer Resistance Protein (BCRP), encoded by Adenosine triphosphate (ATP)-binding cassette subfamily G member 2 (ABCG2), and tested whether they reverse drug resistance in vitro and increase exposure to a BCRP substrate in vivo. The study also highlights important limitations and the need for caution when considering clinical applications.
Background
Why do some medicines fail just when patients need them most? One reason is BCRP, an ATP-driven efflux pump that lowers intestinal drug absorption, limits tissue penetration at barriers like the brain and placenta, and speeds drug elimination, altering efficacy and side effects. Diet-derived flavonoids are widely consumed, and some can block BCRP, but their specific inhibitory patterns and practical impact remain unclear. Understanding which flavonols inhibit BCRP, and how strongly, matters for real-world issues like chemotherapy resistance and statin exposure. The central question: can selected flavonols overcome transporter-mediated resistance and boost exposure to BCRP substrates without undue toxicity? Further research is needed to link these mechanistic findings to clinical use and to clarify the impact of species differences and the low oral bioavailability of flavonols observed in this study.
About the study
Flavonol screening was performed in Madin-Darby Canine Kidney II (MDCKII) cells stably expressing human BCRP and MDCKII-mock controls, maintained in Dulbecco’s Modified Eagle’s Medium (DMEM) with Fetal Bovine Serum (FBS), Nonessential Amino Acids (NEAA), and penicillin/streptomycin at 37°C in 5% carbon dioxide (CO₂). BCRP activity was quantified by a prazosin accumulation assay in Hanks’ Balanced Salt Solution (HBSS) buffered with 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES). Compounds were screened at 2 μM, and anything that blocked activity by more than 25% moved on to half-maximal inhibitory concentration (IC50) testing over 0-30 μM. Dimethyl sulfoxide (DMSO) at ≤1% was the vehicle, with novobiocin as the positive control. After dosing, cells were rinsed with Phosphate-Buffered Saline (PBS), lysed with Triton X-100, and the analytes were quantified by High-Performance Liquid Chromatography (HPLC).
Resistance reversal was tested by exposing MDCKII-BCRP and mock cells to SN-38 with or without each of 14 potent flavonols (5 μM). Viability was measured using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), and reverse fold (RF) and half-maximal cytotoxic concentration (CC50) values were calculated. The total reverse fold (RFt) is defined as the ratio of CC50 in BCRP-overexpressing cells to CC50 in mock cells (RFt = CC50 BCRP / CC50 mock), and is used to quantify the degree of resistance reversal. Molecular docking used the BCRP crystal structure (Protein Data Bank (PDB) ID: 6ffc) via CB-Dock2, with interactions visualized in BIOVIA Discovery Studio and key structure-activity features summarized.
In Sprague-Dawley (SD) rats, the pharmacokinetics of oral sulfasalazine (2 mg/kg) were measured when given alone or co-dosed with 3,4′-dimethoxyflavone or 3,6,3′,4′-tetramethoxyflavone (each 5 mg/kg). All procedures complied with the Institutional Animal Care and Use Committee (IACUC) guidelines. Plasma concentrations were quantified by liquid chromatography–tandem mass spectrometry (LC–MS/MS) using positive electrospray ionization (ESI+) and multiple reaction monitoring (MRM) with an internal standard (IS). Reported parameters included area under the plasma concentration-time curve to last quantifiable time (AUClast), area extrapolated to infinity (AUCinf), maximum concentration (Cmax), time to maximum (Tmax), and terminal half-life (t½). The use of sulfasalazine as a model BCRP substrate in rats enables assessment of intestinal transporter inhibition, although it does not address systemic chemotherapy resistance in vivo.
It is important to note that, in vivo, only sulfasalazine (a model BCRP substrate) was tested, not a chemotherapy drug. Therefore, the reversal of chemotherapy resistance by flavonols was only demonstrated in vitro.
Study results
Screening revealed that BCRP actively effluxed prazosin; prazosin accumulation fell 69% in MDCKII-BCRP versus mock cells, while novobiocin restored levels, validating the model. Of 77 flavonols tested at 2 μM, 22 inhibited BCRP by more than 25 percent; the strongest was 3,4′-dimethoxyflavone (62 percent inhibition), with several methoxy- and hydroxy-substituted analogs also potent. The hit list progressed to IC50 determination: 14 flavonols showed IC50 values below 5 μM, led by 3,4′-dimethoxyflavone (IC50 approximately 1.62 μM) and 3,6,3′,4′-tetramethoxyflavone (IC50 approximately 1.69 μM).
Functionally, BCRP overexpression increased the CC50 for SN-38 from 0.634 to 13.5 μM, consistent with transporter-mediated resistance. Adding select flavonols (5 μM) largely erased this gap: six compounds, including 3,7,3′-trihydroxyflavone, 3,4′-dimethoxyflavone, 4′-hydroxy-3,7,3′-trimethoxyflavone, quercetin (3,5,7,3′,4′-pentahydroxyflavone), 3,6,3′,4′-tetramethoxyflavone, and retusin (5-hydroxy-3,7,3′,4′-tetramethoxyflavone), reduced CC50 in MDCKII-BCRP cells to mock-like levels, indicating near-complete reversal. Others produced partial reversal, reflected in total reverse fold (RFt) values depending on structure.
Molecular docking backed up the lab results. All 14 potent inhibitors sat in the same pocket of BCRP and bound tightly (affinity less than or equal to minus 8.5 kcal per mol). Frequent contacts included pi-stacking with Phenylalanine at A432 and B439, plus hydrogen bonds with Threonine at A435 and Asparagine at A436. Hydrophobic interactions with Valine at B546 and Methionine at B549 further stabilized the complexes. Adding hydroxyl groups favored hydrogen bonding (for example, quercetin), while adding methoxy groups favored hydrophobic and pi-alkyl contacts (for example, 3,3′,4′-trimethoxyflavone). A balanced pattern of substitutions, as in 3,5,6,7,3′,4′-hexamethoxyflavone, created diverse and strong interaction networks.
In vivo, co-dosing sulfasalazine with flavonols increased exposure. Versus sulfasalazine alone (Cmax approximately 80 ng/mL; AUClast approximately 183 ng·h/mL), 3,4′-dimethoxyflavone raised AUClast about 1.79-fold (to about 327 ng·h/mL; p less than 0.05) with modest Cmax elevation, while 3,6,3′,4′-tetramethoxyflavone increased Cmax to about 162 ng/mL (p less than 0.001) and AUClast to about 319 ng·h/mL (p less than 0.05), without changing terminal half-life. These rises align with intestinal BCRP inhibition increasing oral bioavailability, a scenario directly relevant to real-world drug-diet interactions (for example, statins such as rosuvastatin) and to oncology, where transporter overactivity can blunt chemotherapy.
However, the plasma concentrations of the tested flavonols themselves were very low after oral dosing in rats, suggesting their primary site of action may be the intestinal tract rather than systemic circulation. This limits their potential to reverse drug resistance in cancers outside the gastrointestinal tract unless their bioavailability can be improved. Additionally, there are significant species differences between human and rat BCRP transporters, and BCRP expression levels in tissues may differ between species. Therefore, caution is needed when extrapolating these findings directly to humans. It is also important for readers outside the field to recognize that preclinical models, while highly informative for mechanism, do not directly predict efficacy or safety in human patients.
Analytically, LC-MS/MS with ESI+ and MRM quantified plasma levels using an IS, enabling noncompartmental parameters: AUClast and AUCinf, Cmax, Tmax, and t½. These pharmacokinetic terms reflect the extent and timing of drug (or inhibitor) presence in blood plasma, which helps clarify the mechanism and magnitude of any absorption-enhancing effect.
Conclusions
Across in vitro, in silico, and in vivo experiments, multiple flavonols inhibited BCRP, reversed SN-38 resistance, and elevated exposure to an oral BCRP probe substrate, which is evidence that diet-derived scaffolds can reshape drug disposition and, potentially, treatment response. Practically, this signals two things: opportunities to enhance bioavailability of under-absorbed therapies, and cautions about unintended drug-flavonoid interactions. Key limitations include the low oral bioavailability of flavonols, species-specific differences, and the fact that in vivo reversal of chemotherapy resistance was not demonstrated. Future priorities include improving systemic exposure of lead flavonols, testing transporter effects with clinically used anticancer agents, and validating benefits and safety in people, so clinicians and patients can harness BCRP modulation rather than be blindsided by it.
Journal reference:
- Lee, KR., Kang, MJ., Kim, M.J., Im, Y., Jeong, H.C., & Chae, Y.J. (2025). Inhibition of breast cancer resistance protein by flavonols: in vitro, in vivo, and in silico implications of the interactions. Sci Rep. 15. DOI: 10.1038/s41598-025-13908-1, https://www.nature.com/articles/s41598-025-13908-1