The choroid in the eye is part of the uveal tract. This is made up of the colored iris, the ciliary body, and the choroid. All are rich in melanocytes, the specialized cells that produce melanin. This pigment is a dark-colored, light-absorbing particle.
A melanoma is a tumor which arises from these cells. Melanomas of the eye may be anterior (of the iris) or posterior (of the choroid or ciliary body).
Most of these are choroidal melanomas, which are the most common primary intraocular malignancies. The incidence is 6 per million in the USA.
The choroid is a dark layer that underlies the retina, the neurosensory layer of the eye. Most uveal melanomas are choroidal in origin. Choroidal melanomas typically appear as brown, elevated dome-shaped tumors in the subretinal space with associated retinal detachment, especially if the tumors are over 4 mm in diameter. However, the color may range from totally colorless or amelanotic (rare) to deeply pigmented (most commonly).
Symptoms
Choroidal melanomas are usually asymptomatic or silent tumors. In a few cases, the tumor may impinge on the lens or the fovea, or cause retinal detachment, all of which result in decreased visual acuity or blurring of vision. Most often they are detected during a routine eye examination.
However, sometimes their enlargement may cause retinal detachment, with blurring of vision or decreased visual acuity. Serous detachment occurs at times. Another complication is secondary glaucoma which arises due to closure of the drainage angles by extensive detachment of the retina.
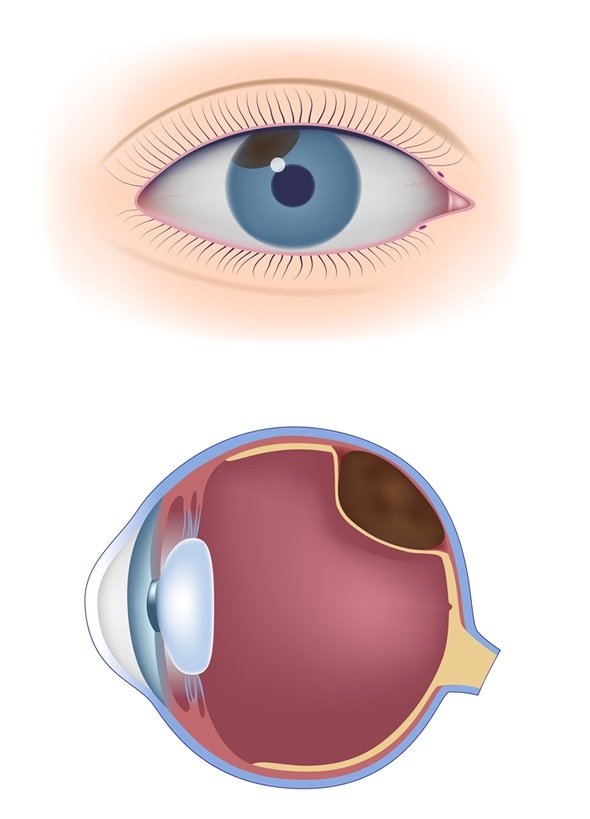
Uveal melanoma - Image Copyright: Alila Medical Media / Shutterstock
Risk Factors
The following factors increase the risk of developing a choroidal melanoma:
- Fair skin
- Blond or red hair
- Blue or green eyes
The incidence of these tumors is higher at older ages. It is also high in individuals with the following conditions:
- Atypical nevus
- Dysplastic nevus syndrome
- Melanocytosis, either ocular or oculodermal
- Certain genetic mutations
Diagnosis and Management
In most choroidal melanomas, the lack of symptoms means that they are detected during a detailed dilated eye examination. Indirect ophthalmoscopy is the most important tool in the evaluation of suspected choroidal melanomas. This is combined with slit lamp examination and gonioscopy.
Uveal melanomas may mimic benign nevi. When they are small, observation may be preferred to watch for progressive growth, which is the mark of a melanoma. Larger tumors require careful examination, especially for the following signs which indicate a higher risk of malignancy:
- Tumor more than 2 mm thick
- The presence of subretinal fluid
- Vision-related symptoms
- The presence of orange pigmentation (lipofuscin) on the surface of the lesion
- The tumor margin is in contact with the optic nerve head in front
Since both a choroidal nevus and an early choroidal melanoma appear similar, a fine needle aspiration biopsy is sometimes taken, especially if treatment is considered necessary. However, the results are by no means infallible. Moreover, there is a risk of seeding malignant cells with this technique. Thus initial observation for the growth pattern of the tumor may be preferred if the melanoma is small and there are no indications of malignant growth.
Other investigations to establish the diagnosis include fluorescein angiography and ultrasonography of the eye. Optical coherence tomography and autofluorescence have also been used. It is important to follow up choroidal nevi as almost 9% of them progress to malignant melanomas within 5 years. At 10 years, this is approximately 13% and at 15 years, about 17%.
The primary treatment for a choroidal melanoma is radiotherapy using a radioactive plaque. This technique involves suturing a small gold carrier containing radioactive seeds to destroy the tumorous cells. For more advanced tumors, enucleation of the eye is required, with postoperative radiotherapy if indicated by pathologic and clinical findings.
Prognosis
The aggressive nature of a melanoma of the choroid may be predicted using several variables:
- The cellular components, with epithelioid cells having a worse outcome than spindle celled types
- Tumor size
- The anterior extent of the tumor
- Involvement of the ciliary body
- Extraocular spread
- Histopathologic features like mitotic activity and lymphocytic infiltration
The mortality rate goes up with the incidence of recurrence, metastasis, and involvement of the extraocular tissues. Almost 30% of choroidal tumors with metastasis are associated with a fatal outcome within 5 years.
References
Further Reading
Last Updated: Jan 2, 2023