Introduction
Population growth, aging, and comorbidity
Burden of disease
References
Further reading
As a result of an increase in life expectancy, several issues related to longevity and health arise. One of these is comorbidities. Comorbidity is the concurrence of one or more clinical conditions in a single person. Chronic disease occurrence is more common with increasing age. For example, the likelihood of possessing two or more significant conditions is approximated to be 60% by the ages of 75 and 79 years and exceeds 75% between the ages of 85 and 89 years.
 Image Credit: Photographee.eu/Shutterstock
Image Credit: Photographee.eu/Shutterstock
Comorbidity describes the effect of all other concurrent conditions that an individual patient may suffer with, alongside a primary condition of interest. Comorbidities can either be physiological or psychological. In some contexts, comorbidities may often be used to describe two conditions that have a highlighted keyboard of occurring together. For example, depression and anxiety disorders.
The term comorbidity can indicate a condition that exists simultaneously and correlatively with a primary condition. However, some comorbidities may arise independently with another condition. However, it is difficult to determine whether or not two conditions are related as diseases are often multivariate and there are likely to be aspects of both conditions which occur simultaneously and independently as a consequence of one another.
Population growth, aging, and comorbidity
overall, the world population is aging and an important part of this shift towards an elderly population is the development of chronic illness. Due to advancements in healthcare, the proportion of individuals who do not die of acute illnesses, such as infections and disease, is increasing. Consequently, they are more likely to suffer from a chronic illness and are subsequently more likely to develop additional chronic illnesses.
Historically, population growth results from several factors which include advances in medical, technological, and public health provisions which have resulted in the control and treatment of a range of communicable diseases, facilitated the control of pandemics, improved health and sanitation conditions, as well as transformed sectors which are related to public health. This includes the agricultural industry, which has increased the proportion of the world population receiving adequate nutrition.
Concurrently, average life expectancy has increased reaching 78 years in the developed world and 68 years in the developing world. As life expectancy has increased, population growth rates have declined; the decline is explained, in part, by falling fertility rates across the world as well as changes in attitudes towards lifestyle/changes in social norms.
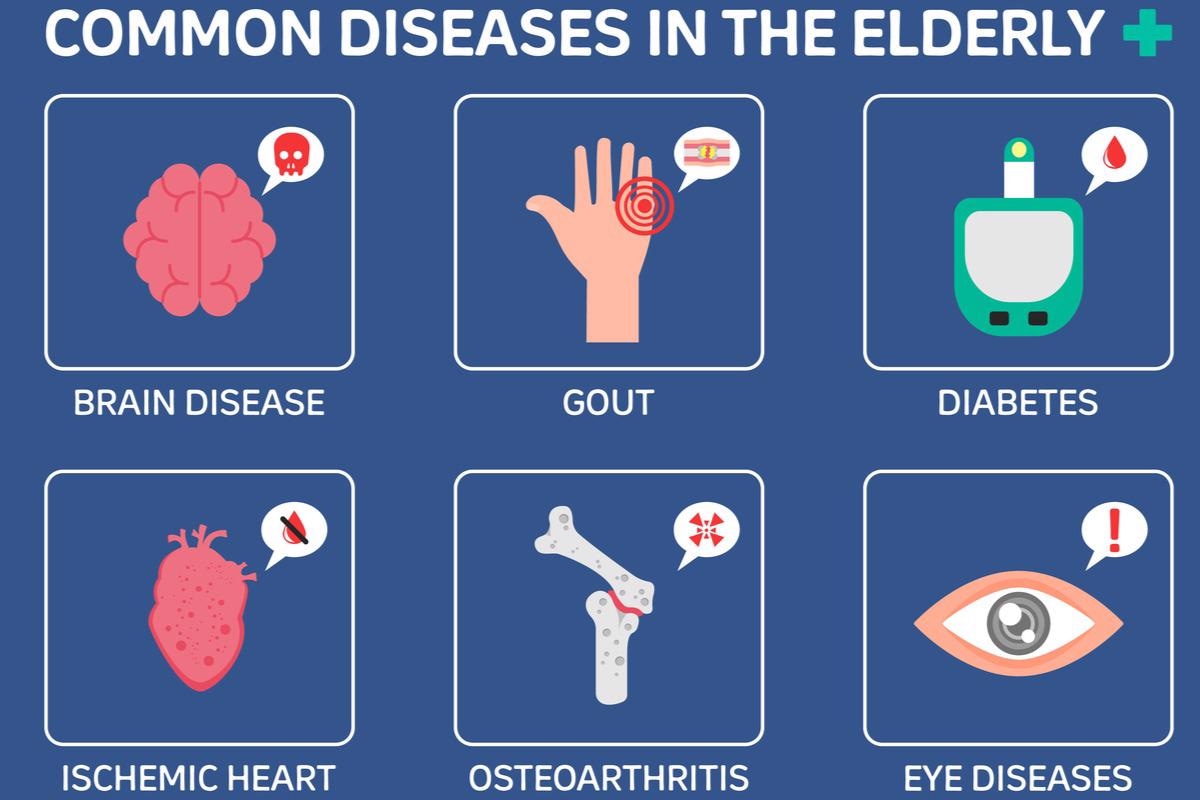 Image Credit: Health Care Vector Life/Shutterstock
Image Credit: Health Care Vector Life/Shutterstock
Burden of disease
Due to an aging population and improvements in healthcare and the diagnosis, treatment, and/or management of disease, many older people suffer from >1 illness. The most common comorbid conditions that occur in elderly people include heart disease, hypertension, respiratory disease, cerebrovascular disease, diabetes, joint disease, sensory impairment, and mental health problems.
Among them, the most common primary condition seen in the elderly is mental disorders, most notably, dementia. This trend of a high prevalence of dementia is seen among the elderly across the world. Quantitatively, low- and middle-income countries (LMICs) make up 62% of all cases, and high-income countries (HICs) comprise the remaining 38%. However, the burden of dementia is increasing, with estimates projecting that the number of cases will rise to 71% by 2050 in LMICs.
Globally, dementia represented the 5th largest cause of death in 2016. Those that suffer from dementia have a high disease burden which involves both cognitive symptoms caused by dementia as well as poor quality of life that results from physical health tolls and medication misuse. As a result, this population suffers from several comorbidities.
Those that suffer from dementia are more likely to suffer from five or more physical comorbid conditions and polypharmacy relative to those that do not suffer from dementia. Polypharmacy is defined as the simultaneous use of several drugs to treat a single or several conditions. It is often associated with adverse outcomes which include mortality, adverse drug reactions, increased length of stay in the hospital, readmission to the hospital after discharge, and increased frequency of falls.
The three most common diseases which are found in those that suffer from dementia include hypertension (34.5 %), diabetes (16.3 %), and cardiac arrhythmia (7.3 %) The prevalence of cardiometabolic conditions is increased for those who have more severe dementia. In addition, comorbidities are considered a risk factor for poor physical and mental health in those that suffer from dementia.
References
- Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005 Aug 10;294(6):716-24. doi: 10.1001/jama.294.6.716.
- National Institute for Health and Care Excellence. Multimorbidity and polypharmacy. Available at: https://www.nice.org.uk/advice/ktt18/chapter/evidence-context. Accessed January 2022.
- Divo MJ, Martinez CH, Mannino DM. Ageing and the epidemiology of multimorbidity. Eur Respir J. 2014;44(4):1055-1068. doi:10.1183/09031936.00059814.
- de Lima JD, Teixeira IA, Silva FO, Deslandes AC. The comorbidity conditions and polypharmacy in elderly patients with mental illness in a middle income country: a cross-sectional study⋆. IBRO Rep. 2020 Jul 16;9:96-101. doi: 10.1016/j.ibror.2020.07.008.
Further Reading
Last Updated: May 31, 2022