Introduction
Epidemiology and outbreak dynamics
Microbiological profile of the pathogen
Clinical features and diagnosis
Public health investigation and source traceback
Recall actions and regulatory response
Comparative analysis with previous egg-linked outbreaks
Implications for clinical and public health practice
Research and policy directions
Conclusions
References
Further reading
The 2025 egg-linked Salmonella outbreak demonstrates how rapid genomic surveillance and coordinated public health action can identify contamination sources, prevent further illness, and inform global food safety strategies.
 Image Credit: R Photography Background / Shutterstock.com
Image Credit: R Photography Background / Shutterstock.com
Introduction
In June 2025, a multistate outbreak of Salmonella enteritidis was attributed to contaminated shell eggs distributed by the August Egg Company based in California. To date, this outbreak has resulted in 79 confirmed cases and 21 hospitalizations, with no reported fatalities.
The United States Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) have traced these infections to eggs produced at the company’s facility, where environmental samples matched the outbreak strain. This incident highlights the ongoing public health challenge of foodborne pathogens, diagnostic readiness, and surveillance of resistance.1
Epidemiology and outbreak dynamics
The current multistate outbreak of Salmonella enteritidis has affected at least nine states across the US between February and May 2025. Most patients reported eating eggs or dishes containing eggs prior to experiencing symptoms.
PulseNet and CDC data confirmed the outbreak strain, which matched environmental samples obtained from the egg production facility. The exposure period aligns with the product distribution timeline, highlighting the importance of rapid detection and response in foodborne outbreaks.
 Pathogenic Salmonella bacteria illustration: Image Credit: nobeastsofierce / Shutterstock
Pathogenic Salmonella bacteria illustration: Image Credit: nobeastsofierce / Shutterstock
Microbiological profile of the pathogen
Salmonella enterica is a bacterium responsible for Salmonella enteritidis, the second leading cause of foodborne illness in the United States. Salmonella, typically found in contaminated poultry products, is highly adapted to colonize the reproductive tracts of hens, thereby enabling vertical transmission directly into developing eggs.
The Salmonella bacterium has evolved numerous specialized virulence genes that facilitate its survival inside host cells and its ability to evade immune defenses. Several genes have also emerged to confer antibiotic resistance to tetracyclines, sulfonamides, chloramphenicol, and aminoglycosides.3
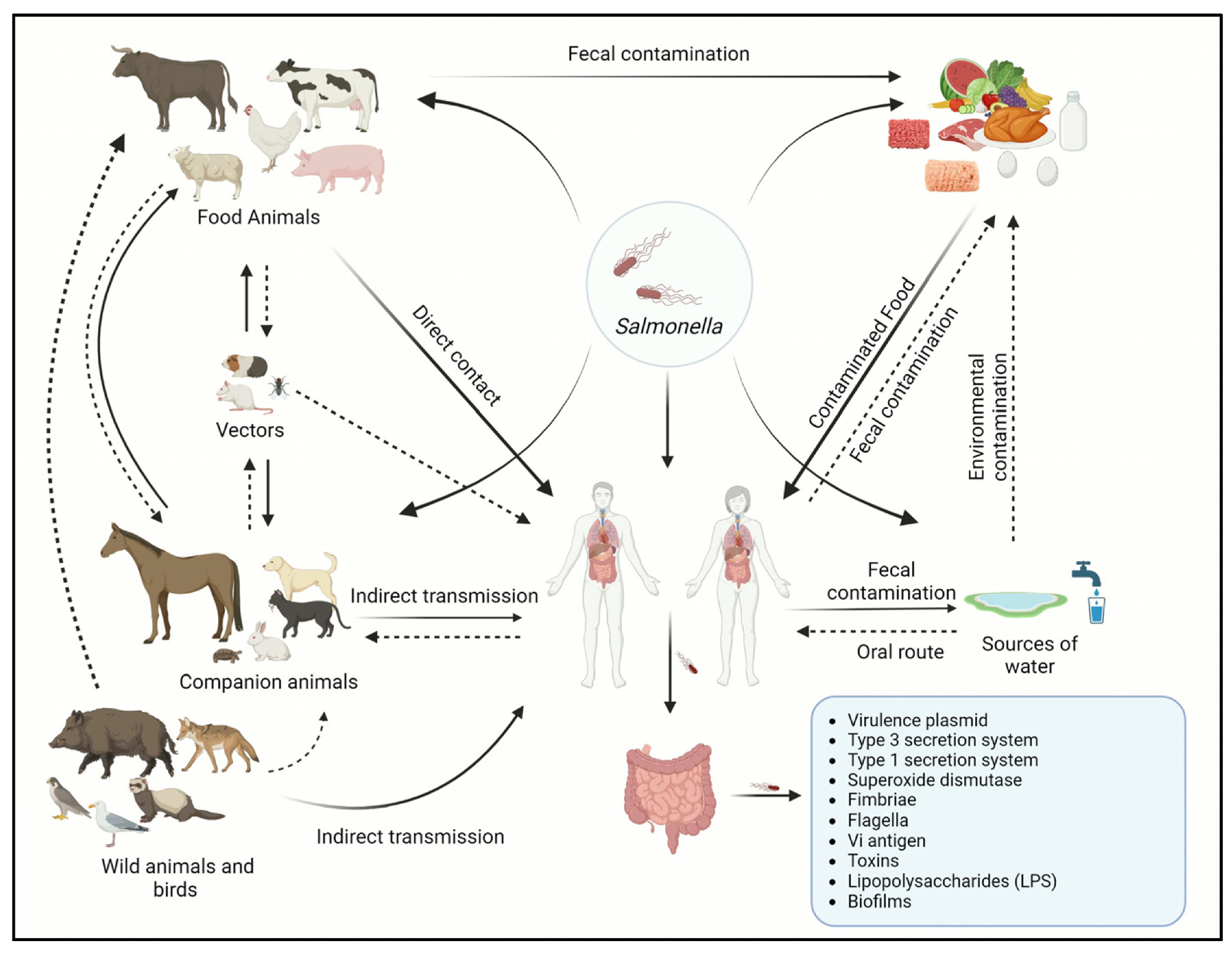 Transmission cycle of Salmonella between animals and humans.2
Transmission cycle of Salmonella between animals and humans.2
Clinical features and diagnosis
The symptoms of Salmonella infection typically arise between six and 72 hours after consuming contaminated food or water, the most common of which include diarrhea, abdominal cramps, fever, and nausea. In some cases, especially in vulnerable individuals like older adults, infants, or immunocompromised, Salmonella infection can lead to serious complications such as dehydration, bacteremia, and extraintestinal spread to organs like the liver or spleen.
Diagnosis is confirmed by measuring bacteria isolated from fecal samples through polymerase chain reaction (PCR)-based assays. Serotyping can also be performed to identify the specific Salmonella strain responsible for the infection.2,3
Public health investigation and source traceback
In response to the recent multistate outbreak of Salmonella enteritidis, the CDC and FDA, as well as state and local health officials, have coordinated a joint investigation. Using whole-genome sequencing and traceback data, investigators identified the August Egg Company in California as the source of contamination, specifically at the production or packing facility.
Environmental samples collected at the site matched the strain associated with the outbreak. This incident highlights the critical role of traceability tools and interagency cooperation in quickly identifying sources of contamination, which have been optimized following previous outbreaks involving eggs and other high-risk foods.1
Major egg recall as salmonella outbreak sickens dozens
Recall actions and regulatory response
In response to the recent multistate Salmonella enteritidis outbreak, the August Egg Company voluntarily recalled 1.7 million dozen eggs with sell-by dates between March and June 2025. The recall affected multiple brands sold throughout national retail chains, including Walmart and Safeway.
The US Department of Agriculture's Food Safety and Inspection Service (USDA-FSIS) and the FDA initiated inspections and follow-up audits at the processing facility. The company diverted fresh eggs to a pasteurizing facility and paused retail sales.1,4
Comparative analysis with previous egg-linked outbreaks
In comparison to previous incidents in 2020 and 2024, where standard traceback methods were often slow and reactive, the recent Salmonella outbreak utilized whole-genome sequencing, which accelerated the rate at which public health officials were able to identify the source of the outbreak. By analyzing the genetic fingerprint of the bacteria, health officials quickly connected human infections to the August Egg Company’s facility.3,5
Similar to reports in China’s Guizhou Province, where two-thirds of foodborne Salmonella strains exhibit resistance to multiple antibiotics, the current outbreak demonstrated that resistant bacteria are increasingly emerging in eggs and poultry. The overuse of antibiotics worldwide is directly implicated in exacerbating antibiotic resistance, underscoring the importance of improving antibiotic practices and monitoring systems, including genetic testing, to protect global food supplies.3,5
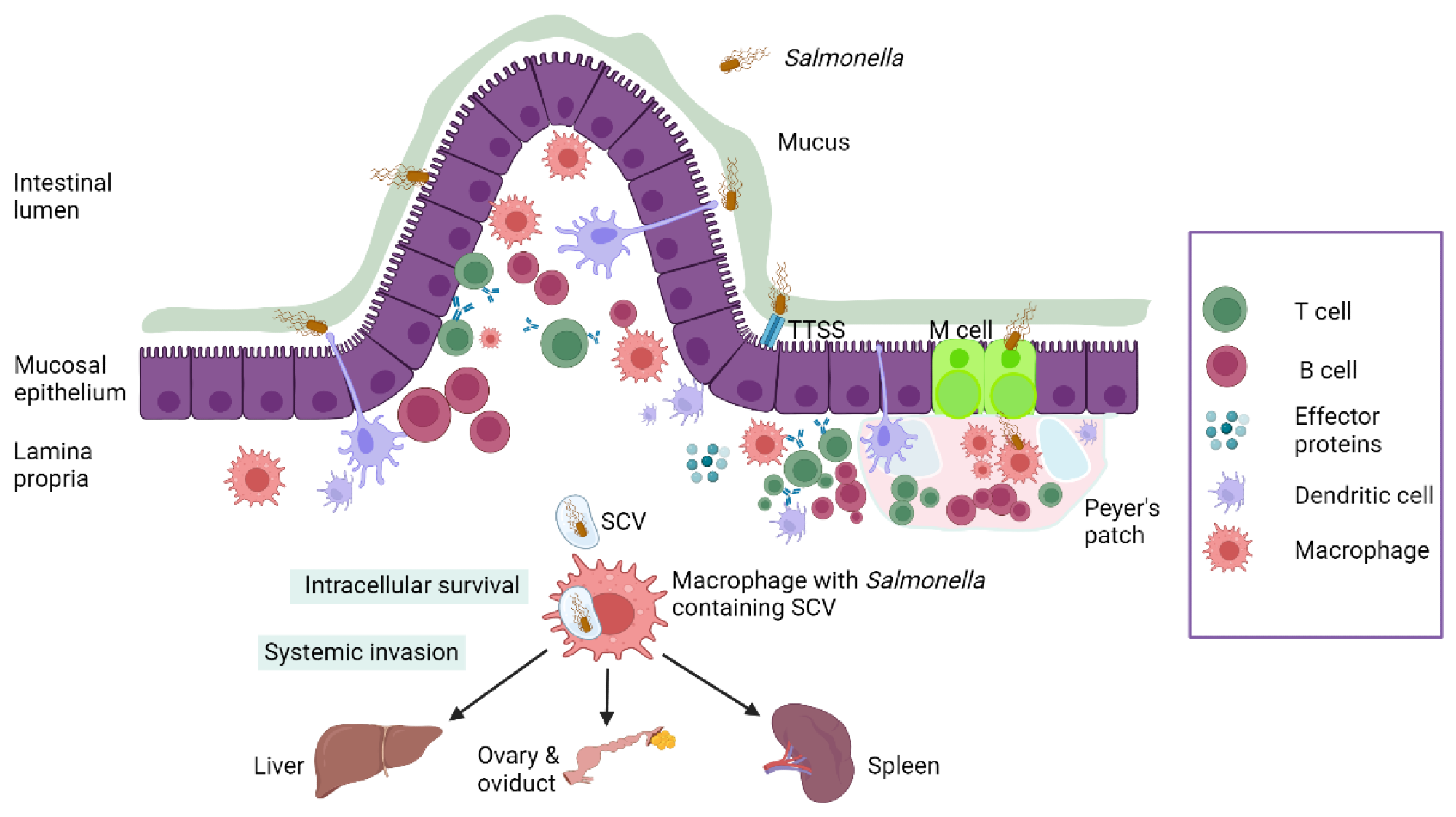 Schematic representation of Salmonella pathogenesis in poultry.3
Schematic representation of Salmonella pathogenesis in poultry.3
Implications for clinical and public health practice
Timely reporting by clinicians during foodborne outbreaks is essential to initiate swift public health responses. Early identification of cases enables public health officials to quickly pinpoint contamination sources and implement rapid interventions to prevent further spread. Clinician awareness plays a vital role in recognizing symptoms and linking them to potential exposure, especially in vulnerable populations such as older adults, those with immunocompromised, and children under five years of age.6
Empiric treatment decisions during outbreaks must be guided by local resistance patterns and updated surveillance data. As multidrug-resistant pathogens become more common, continuous monitoring of antimicrobial susceptibility is necessary to ensure effective therapy. Without accurate resistance tracking systems, treatment failures and prolonged infections are likely to increase.6
From a public health perspective, improving food safety regulations is critical. Policies that mandate egg pasteurization and stricter hygiene standards in the production and distribution of these foods can significantly reduce contamination risks.
Reducing the overuse of antibiotics in agriculture and promoting cross-sector collaboration among healthcare, veterinary, and food safety professionals are crucial steps toward minimizing outbreak risks and preserving the efficacy of antibiotics.6
Research and policy directions
Future research should prioritize strategies to prevent the vertical transmission of Salmonella in poultry, while also focusing on vaccination programs and biosecurity in breeding operations. Real-time tracking using next-generation sequencing can significantly improve outbreak responses and pathogen traceability.
These efforts align with the One Health framework, which integrates human, animal, and environmental health. Addressing zoonotic threats through the One Health approach enables early detection and targeted interventions.
Policymakers are encouraged to support interdisciplinary collaborations and invest in surveillance technologies, as emphasized by international One Health initiatives. These coordinated strategies are crucial for reducing antimicrobial resistance and ensuring sustainable food safety and global health security.7
Conclusions
The recent Salmonella outbreak underscores the clinical and public health importance of rapid detection, effective reporting, and interagency coordination in managing foodborne illness. Clinicians play a crucial role in early diagnosis, timely notification, and guiding appropriate treatment, particularly amid the rising rates of antibiotic resistance.
This incident reinforces the urgent need for ongoing food safety vigilance, encompassing stringent production standards, regular inspections, and targeted public education. Moreover, the outbreak highlights the broader significance of integrated infectious disease surveillance systems that connect human health, veterinary practices, and environmental monitoring.
References
- Outbreak Investigation of Salmonella: Eggs (June 2025) US Food & Drug Administration, June 5, 2025. https://www.fda.gov/food/outbreaks-foodborne-illness/outbreak-investigation-salmonella-eggs-june-2025
- Lamichhane, B., Mawad, A.M., Saleh, M., Kelley, W.G., Harrington, P.J., Lovestad, C.W., Amezcua, J., Sarhan, M.M., El Zowalaty, M.E., Ramadan, H. and Morgan, M., 2024. Salmonellosis: an overview of epidemiology, pathogenesis, and innovative approaches to mitigate the antimicrobial resistant infections. Antibiotics, 13(1), 76. DOI: 10.3390/antibiotics13010076, https://www.mdpi.com/2079-6382/13/1/76
- Shaji, S., Selvaraj, R. K., & Shanmugasundaram, R. (2023). Salmonella Infection in Poultry: A Review on the Pathogen and Control Strategies. Microorganisms 2023, 11, 2814. DOI:10.3390/microorganisms11112814, https://www.mdpi.com/2076-2607/11/11/2814
- August Egg Company Recalls Shell Eggs Because of Possible Health Risk, US Food & Drug Administration, June 6 (2025) https://www.fda.gov/safety/recalls-market-withdrawals-safety-alerts/august-egg-company-recalls-shell-eggs-because-possible-health-risk
- Zhou, L., Ye, Q., Zhou, Q., Wang, J., Li, G., Xiang, J., ... & Li, S. (2024). Antimicrobial resistance and genomic investigation of Salmonella isolated from retail foods in Guizhou, China. Frontiers in Microbiology, 15, 1345045. DOI:10.3389/fmicb.2024.1345045, https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1345045/full
- Manyi-Loh, C., Mamphweli, S., Meyer, E., & Okoh, A. (2018). Antibiotic use in agriculture and its consequential resistance in environmental sources: potential public health implications. Molecules, 23(4), 795. DOI:10.3390/molecules23040795, https://www.mdpi.com/1420-3049/23/4/795
- Osterhaus, A.D., Vanlangendonck, C., Barbeschi, M., Bruschke, C.J., Christensen, R., Daszak, P., de Groot, F., Doherty, P., Drury, P., Gmacz, S. and Hamilton, K. (2020). Make science evolve into a One Health approach to improve health and security: a white paper. One Health Outlook, 2, 1-32. DOI: 10.1186/s42522-019-0009-7, https://onehealthoutlook.biomedcentral.com/articles/10.1186/s42522-019-0009-7
Further Reading
Last Updated: Jun 18, 2025